Crossing the Language Barrier of Pain Scales: #Rheum Blog Carnival
 If you either live with or study a rheumatological disease, then you know that pain is a ubiquitous symptom and an essential factor in evaluating disease activity. “Pain is a most important indicator of clinical status in rheumatoid arthritis (RA),” Arthritis and Rheumatism. While pain is the most obvious sign that something is not right, it is the least obvious to observers. And that can be a barrier to receiving needed care.
If you either live with or study a rheumatological disease, then you know that pain is a ubiquitous symptom and an essential factor in evaluating disease activity. “Pain is a most important indicator of clinical status in rheumatoid arthritis (RA),” Arthritis and Rheumatism. While pain is the most obvious sign that something is not right, it is the least obvious to observers. And that can be a barrier to receiving needed care.
Researchers have learned that quantitative pain assessments are extremely valuable in routine rheumatology care. “Quantitative data concerning pain cannot be obtained from any source other than the patient. Quantitative assessment of pain at each visit in routine rheumatology care, along with the assessment of functional disability, global status, and other patient variables, using a patient self report questionnaire might lead to improved patient care,” Clinical and Experimental Rheumatology.
Pain scales (quantitative pain assessments) are troublesome
Reading questions about pain scales from Jackie and others, I realized that exploring pain scales with rheumatological diseases is a subject which needs a lot more attention. So, when my elder daughter got home from college, she worked with me to create a pain scale image that suggests adding relatable events would be better than just frownies (un-smilies) or the numbers 1 through 10 of a visual scale.
Meanwhile, it occurred to me, “When else do we ask people to just point to something in order to communicate?”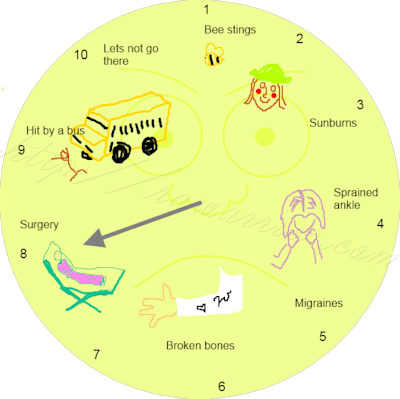
- Toddlers might point when they don’t know the words to use.
- When there is a language barrier.
Come to think of it… Both are true with pain scales!
- We need better language to use to communicate pain levels.
- There is a language barrier with regard to pain.
So I wrote about problems with pain scales and asked others to blog about their ideas!
How can we cross the pain scale language barrier and better communicate? Let’s hear from the experienced users of pain scales! I hope you’ll visit each post!
Lauren at Unguided Missile wrote Pain Scales. How many times has my family heard me say, “If only pain were a color”? If anyone has ever wished pain could be seen, they will love Lauren’s post. She hits the nail on the head again simply: “It’s not so simple as how much it hurts. It’s how much does the pain take away from your life.” This is what I’ve said over and over again to both of the rheumatologists I’ve had. #TruDat
Cassandra at Beauty for Ashes wrote Pain Scales… Why We Love to Hate Them. Cassandra describes why it’s difficult for those with rheumatic diseases to explain pain to friends or doctors, even using specially designed pain scales. “What if you have been in severe pain for so long that your body doesn’t process it the same anymore… you may say you’re only at a 2 when anyone else would say the same amount of pain is a 7!” However, she points out that pain scales could be useful to track the experience of a single patient, especially if they’re used regularly or between medical appointments. When “our physicians understand the differences in our individual cases, scales to rate the pain can be useful.”
Jodi at Aim for Perfection Editing wrote How Do You Edit Pain? Jodi says we should consider editing the pain scale or in fact “DELETE” it! While I understand the need for measuring disease activity, I was moved by her plea for compassion; it reminded me of my wondering whether doctors should love patients. Jodi wrote: “I think the physician should treat each patient with real compassion and concern. Instead of having us fill out a chart of meaningless numbers, sit down and talk to us. Ask me what I do each day. Ask me how my pain hinders those activities. Ask me my specific concerns. Ask me how I manage. Ask me things that relate to my ability to live my daily life, and listen to what I have to say.”
Dana of At the Water’s Edge wrote Rate Your Pain. Dana distinguishes between “soreness” and being “in pain;” also she separates the issue of the constancy of pain. She offers a diagram to help us distinguish the various components that contribute to pain. This is an excellent step. Improving communication about pain is the heart of the matter.
Note that like many others, including yours truly, Dana used a “9” to rate the worst pain she ever experienced, regardless of its medical implications, as if “10” means “Don’t go there.” She moderated her answer as if she assumed that “10” is an answer that is considered unreasonable.
Linda at Rheumatoid Arthritis –Combating Pain wrote Need For a Accurate Pain Scale For RA. Linda recommends The Comparative Pain Scale by Jack Harich. She believes that rheumatologists and medical professionals could certainly assist us better if there were better ways to communicate about our pain.
Jennifer at The RA Vegan wrote Thoughts on Pain Scales and RA. Jennifer’s pain scale adds words to the numbers one through ten, to add significance to each level. One significant thing to notice is that her “one” is a level of pain that is low enough to ignore. It is not pain-free. Pain-free could be zero, but some level of pain is assumed which seems typical of people living with RA. Her pain scale is written in terms of her mothering experience, but as she explains, it is still about pain because of the way that “the pain I deal with impacts my life.”
Jeanette at Renplus wrote It’s all in your head — NOT! Jeanette explains the frustrations with communicating pain: it’s usually invisible and many people have difficulty communicating about it. She suggests that communication is the solution to the imprecision and subjectivity of pain measurement: “People need to communicate to their medical professionals completely and honestly how they feel. Medical professionals need to document the patient’s communication and ask for clarification with compassion.”
Megan at Objects in Mirror are Closer than They Appear wrote (Almost) Wordless Wednesday: Pain Scale for the Vain Girl. She created a visual pain scale called “Pain Scale (through Shoes).” She agrees with others who remind us that those of us with a “continuous level of pain” often develop a “new normal.’”
Rachel at A Happier Mommy wrote One Size Fits All. She suggests that pain could be rated with questions better than with numbers. The bottom line is trust and honesty between patients and doctors: “In all honesty, unless you have a doctor who is willing to really listen and get to know you, there is no perfect pain scale. Everyone is different and carries a different pain tolerance and response.”
Kirsten at Not Standing Stills Disease wrote The Medieval Pain Scales. She thinks life might be better without pain scales with “those damn faces mocking your pain.” Her great idea is for a doctor to provide patients with a copy of the pain chart. Then each patient can keep “a general record of your pain for a month or longer before your appointment, according to the chart. Then, when you are asked what you current pain level is, you should be keeping this chart in mind.”
Nicole at The Confirmed Ache wrote Pain Scales. She discusses how important it is to pay attention to the messages of one’s body, especially pain. She suggests patients find a scale they like and use it to help know when it’s time to take medication or seek care: “I would definitely recommend a pain scale, especially for those who are newly diagnosed. I think it’s good to rate your pain and keep track.”
AfternoonNapper at The Afternoon Nap Society wrote On A Scale of 1 to 10, How Would You Rate Your Pain? AfternoonNapper hones in on the problems of subjectivity and relativity of pain: “The healthcare professional doesn’t truly know me, and I don’t know him or her. The healthcare professional can not ask, ‘So how does what you’re feeling now compare to that time I stepped on a rusty nail and had to go get a tetanus shot?’” Like so many of us, partly due to fears about perceptions, she avoids using of the highest pain rating: “I reserve a ten for a pain that I have not yet experienced” even though she has been “cut in half sideways for elaborate bypass surgery.”
Hurt Blogger at The Hurt Blogger wrote Evaluating the 1-10 Pain Scale. Hurt Blogger shares the intellectual process that occurs when she is asked to rate her pain. Like my daughter and I did when we created our pain scale, she provides relatable events for each number on a pain scale. However, she adds this terrific idea: Rheumatologists and pain specialists should have patients complete a worksheet which details personal experiences to which patients relate various pain levels. This can be kept in the front of the chart with updated pain scale replies.
I think this could go a long way toward helping the care-givers know the relevance of the answers patients give. It’s almost like giving them a window into that thought process that occurs in the seconds between the question and the answer: “How do you rate your pain?”
Lene at The Seated View wrote Faces, Earthquakes and Ebola: Making Pain Scales Work in Real Life. Lene addresses the problems with rating pain such as the tolerances we naturally have to pain, the filters we “slap” onto it to reduce its affect on us (brilliant explanation of coping mechanisms), and the different types of pain: “How can you compare the sharp, clean, localized pain of surgery (The Ginsu) with the Dirty Cotton pain of an RA flare?” She compares various visual pain scales, her favorite being those which relate the way the pain interferes with one’s life.
Tanya of Tanya Martin wrote RAD Pain Scale – Take One. Tanya created her original pain scale for Rheumatoid Autoimmune Disease (RAD) aka Rheumatoid Arthritis (RA). She created a chart that is customized to the types of pain experienced with RA. It is also customizable to specific patients. “I put an example of something they may write to allow family members to see what help they may need during those levels of pain. They may not be able to communicate or think clearly enough ask.” (Click on her chart to enlarge image.)
Amanda at Amanda Gibson wrote Pain Scales. It was a late entry, but I wanted to include it since it has more good advice about communication.
What have we discovered about pain scales?
- Communication is the crucial issue. Better communication about pain levels will lead to better medical care.
- Communication is improved by honesty, trust, and accuracy by each party, patient or care-giver.
- Comparing one person’s responses to another is probably less helpful than comparing the same person’s answers over time.
- Rating pain in the office with a pain scale on a single day, as Jackie said in her question, does not give a complete picture of a person’s pain.




This is awesome. I wish I’d known about this carnival ahead of time. Yes, everyone I know with chronic pain hates pain scales. One of my favorite posts ever was Hyperbole and a Half — her new, improved pain scale is hilarious.
Also, so true about 10! I’ve been in the ER to get morphine and rated myself an 8, or when pressed, a 9. However, I clearly remember one time that was, in my mind, a 10. But I was alone — nobody to tell! But I think I can never call anything else a 10 unless it meets or exceeds that night.
Kelly,
I believe this is just the very beginning of a more global conversation on patients living with chronic pain. Given all of the examples provided in the blog carnival, I wonder if there’s one pain scale or representation that might serve as a current gold standard? And if not, is it possible to use this pain carnival as a starting point to crowdsource a pain scale or representation supported by the majority of this community of readers? If so, then such a pain scale should be adopted for more universal use in doctor’s offices and pain clinics across the country/around the globe.
Additionally, I think it’s hight time the American Pain Society and other organizations devoted to solving “The Problem of Pain” (cf C.S. Lewis) begin inviting pain patients to their annual meetings, like other health organizations have started to do. Maybe the RheumPF can begin to lobby for this as part of its overall mission. Nevertheless, it’s up to all patients in pain to not wait for assistance in the matter but take every opportunity to relieve physical suffering in as many ways as possible. This blog carnival is a major step forward in that direction.
Thanks to all who submitted posts, and to Kelly for organizing for the common good!
-Bob
I stuff pain…I TRY to ignore pain…I don’t own up to pain…not because I’m some sort of super hero, it’s just that I get So tired of trying to explain living day in and day out with some sort of pain AT ALL TIMES. Really, how does one put that on a scale? How can others (esp. care givers) really understand unless they have a situation that’s similar? I guess pain charts are a necessity, but truly, do they even have meaning? Maybe this hour I can move OK. It may hurt like say, a mildly twisted ankle. But maybe 3 hours from now, for some mystic reason, the pain feels more like a broken bone. Maybe my hands don’t hurt so much but my ankles are killing me…If anyone has any good ideas on that, I’ll really like to hear! This pain thing is so dang difficult!
Hi dldg,
I’ve had RA for 4 yrs., been in a continual flare since diagnosis and my caregiver who happens to be my husband was the only person I felt really understood the reality and the depths of my pain. Last year I had shingles 3 times. Shingles is a very painful condition, but I didn’t even know I had it the first time until I was at my regular rheumy appt. and he was listening to my lungs and he said “Do you know you have shingles, you have a patch about the size of a softball that is solid blisters on your right shoulder blade”. I had felt some pain there, but is was nothing special compared to the rest of my chest/rib pain with each breath. I had at least a hundred blisters before it was over and during that year they recurred twice. Last month my wonderful, care-giving husband got shingles and I have listened to HOURS of his side of phone conversations as he tells everyone who will listen about the unbearable pain of shingles. It is all I can do to keep my mouth shut. He had 6-7 blisters total, I listen to him and think “Do you not see me sitting here? Do you not remember that I had this 3 times and each case was much worse that yours?” So, does anyone other than us ever really understand?
I have the same problem when I go see my rheum The pain and joint/body survey {can’t remember the name} doesn’t mean much to me. You see the dr every 3 mos but my RA flares are continual but variable. So how does one demonstrate this on the surveys so you get the “points” to really demonstrate how you are doing.
Saw my rheumatologist today, she had me fill out a new functional evaluation. It asked me how much the RA made it difficult to do different everyday tasks. She also asked about pain and swelling, but said that the functional eval helps discover the effects of RA that people might ignore if they simply accept living with pain. For example, I don’t complain much about the first 1 1/2 hours of the day being worse, when I know I have had periods where it was bad all day.
Thanks so much! Once again I found myself thinking, “Where do I go, who gets it?” It helps to read your blog and everyone else’s posts.
I just returned from a “vacation” with my senior mother. It was so hard, really, really hard. The schedule, the hotel, the hard restaurant chairs, and the walking. She is twice my age and it was hard on her but I had to act like I was fine. I wanted to be fine. I have passed more than 20 kidney stones (4 large enough for medical intervention), had gallstones and broken bones, played competitive soccer, gave birth without any pain intervention, sprained an ankle so badly that it looked like a sprained knee, and have suffered with neuropathic pain resulting from a very bad surgery, and had 3 major surgeries in 3 years. But the inside-out, chronic persistence of the RAD pain really puts me beyond the 1-10 smiley-face pain charts. I can’t describe it and I really believe that if you haven’t lived with it you can’t understand it.
I can’t say much more than “Amen,” Lyndsey. And there are numerous similar lists to yours written by patients all over this site!
I think all of y’all are right, we do need a better pain scale for chronic pain patients. Please understand, however, that Donna Wong and her colleagues developed the smiley-frowney-faces pain scale for small children in acute pain, who can’t articulate how they feel. How or why this scale has been adopted for use with adult chronic pain patients, I have no idea. But the suggestions from the participants for new concepts and constructions of pain scales are some of the most innovative I, as a nurse-scientist who has investigated various rating systems for different conditions, have ever seen. Kudos to all who participated! We need to continue working on these until we find a scale that meets the needs of the largest number of RAD people. However, it still needs to have a caveat in large red letters at the bottom to remind health care givers to TALK TO YOUR PATIENT about the selection made from the scale!
I would be glad to be part of a working group of patients to do this. Perhaps my expertise as a nurse can help?
Cheerio!
Elizabeth
Hi Elizabeth, I’ve read several articles/ editorials from the last 25 yrs that show it was a process – a need to measure – and a discussion of what would work best. There are numerous alternatives, but none have been adopted. Check out the 2 links in the post as a good start. I think we ought to continue the discussion as Bob suggested.
Kelly, Donna was a colleague of an associate of mine. I heard all about the development process of the Wong Scale as it was being developed. This was back when there were serious discussions about whether newborns and especially prematures even sensed pain! Children were supposed to not have much pain compared to adults. Donna was convinced that children did experience the same degree of pain that adults did, and developed her scale to prove it. Adults already had the 1-10 scale. Donna’s led to entirely new ways of looking at children’s pain.
As Bob says, we need to start including chronic pain patients in the development of a pain scale to address our needs. We need the same kinds of serious discussions about the kinds of pain, and degrees of pain we experience, how it affects our lives in terms of functionality, flexability, ability to relate to family and friends, ability to work, social life, etc. All aspects of our lives are affected and interfered with by our pain (as all here on this site know). So all the aspects involved in our lives need to be included.
It will take a conference group of patients, professionals and patient/professionals to work this out. Maybe we can get this on the fast track through an ACR research grant. I really, really think now is the time for this. And this Chronic Pain Scale may actually help those of us with RAD to get taken seriously!!
Just sayin’ 🙂
Love
Elizabeth
When you live in chronic pain with RAD and other similar diseases, your body builds a tolerance for pain. It is very hard to describe in numbers. On my next visit to my rheumy, I’ll simply answer “run over by a bus” best describes it. I’ll let you know what reaction I get.
When I saw my new dr for the second time yesterday, I noticed a new pain scale that had comments with the faces. Wish I had thought to ask for a copy of it. And with my crappy memory, can’t remember exactly what it said.
This dr is really a breath of fresh air. Attentive, caring, listens, understands I need a partner in this. Told me how much he appreciates that I do research, how important it is for me to be invested in my treatment. I gave him a copy of Dr Adams article off of here. We talked about the different medicines, I related what I know about the actual patient results. He was surprised I was aware of that. But…like I told him, I will take his advise and give any treatments a good try if it is one he wants me to try. Because hope is the one thing we can’t let go of.
What a wonderful report, Becky. Thanks for sharing!
Those are great points! I guess its hard to know how to compare pain levels, when you don’t know what a level 10 feels like!
Frownies. 🙁 cool. :)I wish pain were visible too… But since its not, those of without RAD ought to have have compassion, and maybe less complaining since others have it so much worse?
This is a great post. All the diagrams and pictorials are fantastic. A few weeks ago I went to a new doctor for my foot and it was the first time a doctor said to me (with out me saying it first!) that it was hard for her to tell how much pain I was in because RA sufferers have such high pain tolerance that their pain scales are way off. I have been saying to folks for years and getting weird looks. It is always good to be validated.
Definitely true on all counts! Thanks for posting. & I’m glad u have a good dr who knows!
I feel quite fortunate that my current rheumatologist has never asked me to fill out a pain scale or to look a happy/sad faces. That process seems such an inadequate way to try to summarize all that RA is and the qualities and intensities of our pain. My appointments are more of a conversation between my doctor and me. We talk about how I am doing, how my pain and stiffness levels have been, and about what challenges I am having, and most importantly, he takes my word for it. I think it would beneficial for ME to keep track of it, however. It might help me see trends that would help inform my care.
Kelly, I suspect an e-mail would do for this, but I wanted to be sure others with interests in pain would have some kind of access to it. I was reviewing a case and found this pain scale developed by a researcher at MD Anderson Center in TX (the famous cancer center). This is a marvelous pain scale, and might do well for Rheumatoid Autoimmune Disease. Here is the link. http://bit.ly/dJ1xAz They charge for commercial use, and for funded academic research. But it is free for non-funded academic research, and individual clinical practice. Y’all take a look and see what you think. There is one change I would make on it, and it may cost something to do that. Maybe ACR could take it and run with it, but rheum docs should see this and we might play with it some.
Cheerio!
Elizabeth
PS – I’m working with Enrique over at http://www.flarewatch.com to help his tool cover rheum and fibro issues (so many of us have fibro, too). It’s a little uneven as yet, but he’s working to make it better and is very open to suggestions.
Cheerie-Bye!
Elizabeth
Hi,
I really have a hard time typing because my fingers don’t go where I want them to most of the time, and it hurts. My last post wasn’t finished or proofread. What I was getting at (and never finished) was since I lost my health insurance in 2010, my RA’s and GP’s seem not to be as interested in treating my symtoms as much as they’re concerned with how much it’s worth to them.
While I was still working and made 70k/year and had BC/BS the doctors I bent over backwords trying to help me feel better and lessen my symtoms.
Now that I’m retired on disability (but not social security) and have no health insurance they seem a lot less enthusiatic about helping me. My present RA doctor doesn’t even ask about my pain. What do you do with a problem like this?
I have had good insurance since I’ve been diagnosed and have never had a dr ask me about my pain or symptoms. Since I have health insurance, I’ve assumed the reason is that they don’t understand – either they assume I’m not very sick because I don’t look very swollen in the office to them or because they don’t understand the disease enough to know how bad it can be for patients who don’t respond to treatments. So MAYBE there is another reason other than money for the way they don’t do much. Hopefully you can find someone better.
What would I do? It can be tough to get good care and even tougher without money. I’d try to get to a university setting if possible – it is usually good care & they tend to have sliding fee scales for payment. Maybe if you can get a treatment plan worked out, you can also get a dr to make sure you have refills with fewer appointments. I’ve also used local health dept services for refills for thyroid dz when I had no insurance. Sometimes docs also run routine tests that don’t give them much info for your treatment but are costly – another way you might be able to save. Some pharma companies also have treatment assistance websites to help with costs.
Pingback: Pain Scales
Pingback: (Almost) Wordless Wednesday: Pain Scale for the Vain Girl | Patient, PhD
I can very well understand this, my granny spent her entire life with a rheumatological disease and it was painful. I think her biggest problem was failed communication. She was never able to convey the degree of her pain.. Well thanks for the post, I am sure it will help others for better understanding.
I really don’t like those pain scales. How do you quantify the relentless demon that comes at you with a hundred faces? Something I heard some doctors do that I like better is asking “how much better do you feel?” That I can relate to … even if the answer is that I feel worse. This is how I’ve been retraining my brain to think about pain levels. =^^=