Rheumatoid Arthritis News Articles, Volume 2
3 hot Rheumatoid Arthritis news articles
1) Woman with Rheumatoid Arthritis dies after seafood
The Galveston Daily News reported last week a Port Bolivar, Texas woman with Rheumatoid Arthritis died of an infection of flesh-eating bacteria. The bacteria, which are common in warm salt water worldwide, can cause necrotizing fasciitis. Ginger Ling, 57, had cleaned and cooked seafood the day before being hospitalized. She had been diagnosed with RA two years earlier.
Officials believe the infection was likely caused by a bacterium called Vibrio which can be contracted by eating raw or undercooked shellfish. According to officials, Vibrio can be treated if caught early. Ling was treated with antibiotics.
“’Certain folks are more susceptible to experiencing problems with it,’ Koopmann said. ‘Those with a compromised immune system, liver disease, diabetes, cancer, any kind of medical treatment that could weaken the immune system.’ Tammy Bage said her mother was a lifelong resident of Port Bolivar and loved seafood. She took steroids since 2008 for rheumatoid arthritis, which had her wheelchair bound, Bage said.”
2) New efforts to protect RA patients from cardiovascular death
 A pilot study looked for ways to eventually predict cardiovascular events in RA patients. Many RA patients die earlier due to the effects of the disease on the heart. Often there are no typical signs of cardiovascular disease (CVD) in people with RA. The CVD of RA does not occur for the same reasons (high blood pressure, tobacco, high cholesterol, stress, excessive alcohol, and obesity) as in non-RA patients and it’s not as easily detected.
A pilot study looked for ways to eventually predict cardiovascular events in RA patients. Many RA patients die earlier due to the effects of the disease on the heart. Often there are no typical signs of cardiovascular disease (CVD) in people with RA. The CVD of RA does not occur for the same reasons (high blood pressure, tobacco, high cholesterol, stress, excessive alcohol, and obesity) as in non-RA patients and it’s not as easily detected.
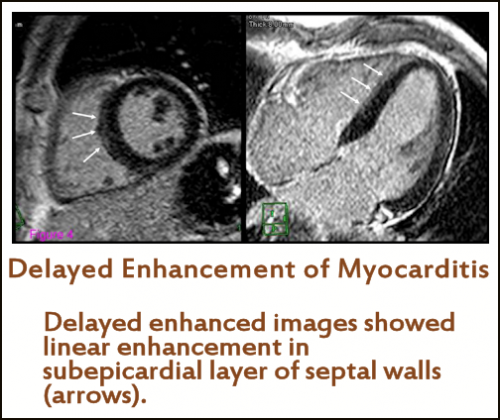
“Rheumatoid arthritis (RA) is a multi-organ inflammatory disorder associated with high cardiovascular morbidity and mortality. We sought to assess cardiac involvement using a comprehensive cardiac magnetic resonance imaging (cMRI) approach and to determine its association with disease characteristics in RA patients without symptomatic cardiac disease.”
There were exciting findings. Abnormalities were indeed found using the cMRI in RA patients who had not had cardiac symptoms: “Myocardial abnormalities, as detected by cMRI, were frequent in RA patients without known cardiac disease. Abnormal cMRI findings were associated with higher RA disease activity, suggesting a role for inflammation in the pathogenesis of myocardial involvement in RA.”
The Arthritis Research and Therapy pdf contains details of the study, charts, references, and images of the cMRI’s.
3) Big news: degenerative disc diseases are related to immune response
Kathryn sent in a fascinating news article fromScience Daily about disc disease. Many of us diagnosed with RA also suffer from degenerated discs. Recent theories about Fibromyalgia syndrome also point to degenerated discs as a source of pain. Look at what researchers found: “Herniated discs occur when the tough outer layer of cartilage cracks, allowing pieces of the softer inner material to protrude into the spinal canal. Until recently, it was thought that pain occurs when the material touches a nerve. Now doctors believe the pain is the result of an immune response caused by the presence of inflammatory cells.”
New information about what causes pain means a lot if you have been told that pain does not have a “real” cause. What if science catches up to pain? What if “inflammatory cells,” of which RA patients have vast amounts, are still being uncovered? Whenever an organic cause can be found, pain may be more treatable.
“The finding implicates the cytokine molecule interleukin-17, and supports the burgeoning theory that an immune response plays a significant role in disc disease, says William J. Richardson, MD, an orthopedic surgeon at Duke. It may also open the door for new, therapeutic approaches that target a specific immune response in hopes of halting disc destruction, and possibly reversing the disease process… By identifying the specific subpopulation of lymphocytes (immune cells that are excited into action by the cytokine), it may soon be possible to arrest the body’s inflammatory response to disc cells,’ says Richardson, senior author of the research published online in the July issue of Arthritis and Rheumatism. Doing so could reduce the painful inflammation associated with degenerative disc disease, and halt the evolution of arthritis. It may also reduce the need for back surgery.”




“The CVD of RA does not occur for the same reasons (high blood pressure, tobacco, high cholesterol, stress, excessive alcohol, and obesity) as in non-RA patients and it’s not as easily detected.”
That’s interesting! I’m a bit concerned though as I already have some factors that contribute to CVD outside of RA. So I guess it’s just another good reason to keep an eye on keeping my heart healthy.
Thanks for sharing, Kelly!
That first item seemed like the RA was just kind of thrown in. Perfectly healthy people die of virulant bacteria too. I was a little confused on the last sentence. Did taking the steroids put her in the wheelchair or was she in a wheelchair because of her RA?
Intersting article on the CVD.
As for disk problems and pain, in my younger days I had a herniated disk due to a mechanical injury. And that pain was definetly due to the bulging disk pressing on the nerve. They cut away the bulge and the pain was gone instantly. With denegerative disk issues and mild bulging, inflammation might play a role in the pain, but if the disk bulges too much then that pain is definetly due to pressure on the nerve. OUCH!
When I read it, I though it was saying that the steroids were the reason her immune system was compromised / weakened which lead to the vulnerability to the infection. These are short summarizies w/out much commentary meant to introduce the news stories that are linked to.
CVD: a doctor I know sent me this this week: http://www.medscape.com/viewarticle/727794?src=mp&spon=27&uac=15348AY I think he was Tweeting/ blogging about CVD of RA also.
Yes, ouch. I have some bulging discs myself. Saw the spine pain man today. Well, I saw the top of his head. This guy never looks up. My spine has OA, RA, bone spurs, and DDD. It is hard to untangle all of the symptoms. But back to the post: The newest theory on FMS is based upon altered pain thresholds and nociception as a result of “polypain” which is shown to have it’s source in widespread OA in combination with ddd. If it’s interesting to you, I recommend the book. It’s linked on the new FMS post.
Kelly, great blog. I think researchers have only scratched the surface of what autoantibodies are present in RA. (and other autoimmune diseases). It would explain why there often isn’t a straight forward positive diagnostic lab for every RA’er, and why not everyone responds to the same RA meds.,esp biologics. The cMRI is interesting. I had a cardiac CT angiogram so I will be looking up the link to see how this differs in the info gained , in each procedure.
Wow! Fascinating articles. I look forward to having time to read the articles you linked to! Thanks for putting it all together in one handy package!
Thanks. 😀
Regarding the last item, IL-17 is not just involved in degenerative disc disease which many of us do have. It is also involved in the synovium in RA joints as the following abstract shows.
“Our data demonstrate a link between the presence of pro-inflammatory Th17 cells in SF [synovial fluid] and local PDUS [power doppler ultrasound] scores, and offer a novel immunological explanation for the observation that rapid joint damage progression occurs in patients with persistent positive PDUS signal.”
PLoS One. 2010 Sep 1;5(9). pii: e12516.
Linking power Doppler ultrasound to the presence of th17 cells in the rheumatoid arthritis joint
http://www.ncbi.nlm.nih.gov/pubmed/20824142
I kept trying to tell my rheumy that I felt there was an inflammatory component to my low back pain. I said this because raising my mtx dose and prednisone doses, or lowering them seems to make a difference in the episodes of low back pain. And it just “feels” inflammatory. I don’t know how much either of these meds has an effect on IL-17, but feel there must be some effect. Hopefully the research to treat low back pain via IL-17 will also bring some relief to autoimmune arthritis sufferers.
Also see this abstract re: Th17 and IL17:
http://www.ncbi.nlm.nih.gov/pubmed/19132915
I had been thinking for some time about the degenerative disc disease aspect and whether it might possibly be RA related. My first spontaneous rupture was in 2002 and my second in Nov 2009. I was especially interested in the artcle I sent to you. I’m so glad that you had chance to read it and include it in your blog.
I don’t know why I still get amazed that so many Rheummys are not ‘up’ with the latest research etc. I mean I shouldn’t be, given not just my own experience – but of so many others both here and on your FB page.
I learn something new every day from you Kelly and the other warriors.
I just pray along with you all that the proverbial ‘they’ make faster advances in finding a cure.
Thanks again, Kathryn. There may be more than one type / cause of ddd, but I sure do meet a lot of RA patients who have it.
This is so interesting – I have the same low back problems. Love the research.