Susceptibility for Rheumatoid Arthritis Acquired via Microchimerism?
Women with RA ask why it’s so common to acquire severe Rheumatoid Arthritis after pregnancy the way I did. I don’t blame my son since my symptoms went back years, but these studies are fascinating…
Rheumatoid Arthritis HLA shared epitope may be acquired in pregnancy
 The current issue of Arthritis and Rheumatism brings a study which concludes that “RA patients who genotypically lack the SE (shared epitope) can acquire the SE as persistent microchimerism from fetal-maternal cell exchange, suggesting that SE-encoding microchimerism could be a risk factor for RA.”
The current issue of Arthritis and Rheumatism brings a study which concludes that “RA patients who genotypically lack the SE (shared epitope) can acquire the SE as persistent microchimerism from fetal-maternal cell exchange, suggesting that SE-encoding microchimerism could be a risk factor for RA.”
An abstract presented last November at ACR examined whether Rheumatoid Arthritis patients can acquire the shared epitope through Microchimerism. From the full study, in this month’s issue: “The quantity of SE microchimerism (microchimerism concentration) was higher in RA patients than in healthy women. Ranked values of microchimerism with the SE overall were significantly higher among women with RA than healthy women… In separate analyses for SE type, the ranked values of QKRAA microchimerism were also significantly higher among women with RA compared to healthy women… Similarly, ranked values of QRRAA microchimerism were significantly higher among women with RA.”
What is the Shared Epitope (SE)?
The shared epitope for Rheumatoid Arthritis is as genetic pattern that is common in RA patients, especially those with CCP antibodies or severe RA disease.
I found a free article on PLoS One which explains the shared epitope for Rheumatoid Arthritis: “The ‘shared epitope’ (SE) is a five amino acid sequence motif in positions 70–74 of HLA-DRβ chains encoded by HLA-DRB1 alleles that are strongly associated with susceptibility to severe rheumatoid arthritis (RA).”
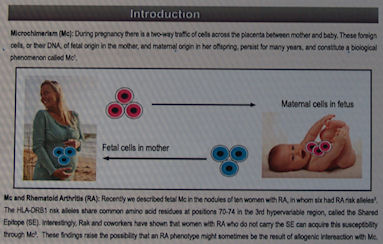
What is Microchimerism?
One of the researchers, Dr. J.L. Nelson, has authored a site devoted to explaining Microchimerism (Mc). He explains that genetic material can pass from mother to child or vice versa during pregnancy, contrary to what some of us were taught in college. Even opposite gender DNA can persist for decades. Dr. Nelson and other scientists have been studying how Mc may relate to autoimmunity.
“Fetal Mc may be beneficial during pregnancy in women with rheumatoid arthritis, as elevated levels significantly correlated with pregnancy-induced amelioration of arthritis.” They also believe it may also be involved in the development of RA since it was detected in Rheumatoid nodules. Their hope would be to either harness its protective tendencies or unlock the process by which may stimulate the onset of RA.
Male DNA in mom’s Rheumatoid Nodules via Microchimerism
We went to the intriguing poster session at the ACR meeting called “The Clinical Features of 13 Women with Microchimerism in Rheumatoid Nodules.” Rheumatoid nodules of 13 women with clinically severe RA disease were found to contain male DNA. We were amazed that there was an inverse relationship between the ACPA (anti-CCP) level and the amount of male DNA.
The SE (shared epitope) risk gene was positive in 10 of the 13 patients and 10 of the 13 sons. They concluded that there is a connection between Microchimerism (Mc) and “citrullination of the SE in the pathogenesis of RA” with a possible function for “microtrauma” and an inverse relationship with anti-CCP.



Not so much a comment as a thank you!
You ROCK! Or more toned down – you are truly a godsend Kelly.
Kinda over my head. What they are saying is we can get the DNA from our baby while in utero and get RA. I wonder if the DNA can stay dormant until years later?
Ronda, I think it says that if we don’t have the genes that make us susceptible to RA that we can acquire them via Mc / during pregnancy, yes. And yes, it can still be years before RA is triggered and the genetic material acquired by Mc can exist for decades.. so a lag time like that sounds reasonable. I have to say that I read this stuff for 2 days before I wrote the post and I still kept exclaiming that it was difficult to comprehend. Seemed important enough though, so I tried.
Hi Kelly, I think you did a good job trying to explain what the paper is trying to show. Let me add a bit more and see if we can make it more accessible.
The shared epitope hypothesis for RA has been around for about 20 years or so. Basically if you have certain combinations of HLA-DRB alleles you’re more or less susceptible for RA, so the theory goes. HLA-DRB is a gene that codes for antigens (different proteins on the cell surface of things like B cells and macropages). Each gene is formed from a pair of alleles (if DNA was a zipper each allele would be one set of teeth). These different alleles have multiple sequences. The shared epitopes are various pairings of different DRBx sequences. Make sense?
In microchimerism, you have cells from another person that take up shop in your body. This can happen in pregnancy when some of the cells from the fetus pass through the placenta. Normally the placenta is a barrier preventing the blood/cells from the mother and fetus to mix. Microchimerism can also happen from things like blood tranfusions or organ transplants.
It isn’t the mother’s DNA that has been altered by the presence of these foetal cells to now have the shared epitope. It is the DNA in the cells of the fetus that live on in the mother that have the shared epitope.
Clear as mud?
No, clearer than mud. More like ocean water. The zipper analogy is great. Thanks. 🙂 I do understand most what you are saying, but probably only because I read hours of background stuff already. Isn’t it odd that the added genetic material would make mom more susceptible to RA? Yet you say her own DNA remains intact. That’s incredible. The presenter at ACR was really excited about demonstrating it w/ the male DNA in women’s nodules.
Well with the male DNA in the synovium of a woman it is pretty convincing evidence of microchimerism.
Yes, the mother’s DNA is unchanged. It is just now you have another persons cells living in your body along side your own cells doing what cells normally do. If the new cells have the shared epitope then they are making the proteins that are thought to be involved with RA.
It’s a pretty cool clue as to where to look.
Thank you Kelly and RaRAP, clearer now and really fascinating. Thank you.
Cool got to love genetics and how many new discoveries will be gleaned from it. makes me miss my biotech work, then I remember the 12 hours days and come to my sences.
Thank you so much Kelly and RaRAP!!!
This is so interesting. So do the fetal cells have some kind of genetic marker for RA? Or just a factor that combined with the mothers cells make RA more of a possibility?
There isn’t anything special about fetal cells in general. Any old fetal cell wouldn’t necessarily have the genetic marker/shared epitope.
This would only happen if the fetal cells have the shared epitope in their DNA.
I would suspect that the mother’s immune system would interact with the proteins made from these genes in the fetal cells. Certain immune cells have a memory of the antigens they’ve come in contact with. Perhaps that is what leads to her developing RA. This would be the same principal behind vaccines. I’m not sure if this holds true for this situation, but it seems plausible.
DNA is a pretty tough molecule. It doesn’t just go around mixing. Honestly I know of no natural process that would allow for the DNA in one cell to mix with the DNA of another. Once the genetic material from the sperm and egg come together and form the DNA sequence it is then fixed and it will be that way for life. We can get gene mutations, but those don’t affect your entire body. Just the cells that have the mutated sequences. Take cancer for example. If gene mutations lead to cancer (most cancer cells have several gene mutations) then only those cancer cells would have that new sequence. Not your entire body.
I guess another way to consider this is that if the mother got cells from the fetus that had the shared epitope, then that would mean her child would have it. I don’t know if that means the child is more likely to get RA or any other related autoimmune diseases or not. I don’t know enough about this gene to know if it is causal or just related.
I mentioned to my Rheum yesterday about this connection. After we discussed what happened when I delivered my son (25 years ago, c-section, 12 days in the hospital, cause of “infection” never found), and the subsequent health issues I’ve had in the last 10 years, he agrees. He is now seeing a clearer picture of my situation. But alas, my CRP is still 1.7
I was talking about this with another scientist and I need to correct something.
The shared epitope isn’t a gene. It is the actual protein. This is the protein/antigen that is recognized by the immune system.
HLA-DRB is the gene that codes for the protein.
All my comments above are mostly correct but I just wanted to clarify so as not to mislead anyone.
Sounds like it could be possible that I got my RA from my husband’s grandpa!
Now that would be an interesting thing to study! :O
Now lets not go around casting blame at distant relatives. I haven’t come across anything to say that the shared epitope is causal. You can get RA or other autoimmune disease without it.
You might have the shared epitope from your own DNA. If you were negative for the shared epitope and you acquired it via microchimerism (the basis of the paper in the main article), then you would’ve acquired it from your child while in utero. Your child has a mix of the genetic code of you and the father of your child and each of you only contribute half of that.
RaRAP, just to be sure you realize – Ronda is a friend of mine & I’m almost certain that we were both 90% sarcastic. People do ask me all the time “where on earth did this come from since there has never been RA in my side of the family?” So this is a remote but plausable thing to explore. I hope I didn’t imply causality anywhere with my lack of sophistication w/ the topic. I’m thankful for the discussion you bring!
Well RA and Type 1 Diabetes both run in my family. I wonder if any of my four children will develop autoimmune disease. And if my developing RA was any indicator of that. But this paragraph really cleared up my questions:
“I would suspect that the mother’s immune system would interact with the proteins made from these genes in the fetal cells. Certain immune cells have a memory of the antigens they’ve come in contact with. Perhaps that is what leads to her developing RA.”
Thank You.
Yes, I was being funny, but it is possible from what you said right? If my child carried it from grandpa Knox and shared it with me to make a match up. That is what I meant. I just found out that my paternal grandmother quite possibly had RA. So this is where it probably came from. I know very little about that side of my family, but I’m beginning to learn having just met some of them on Facebook. Thanks for your explanations RaRAP. I am not happy that my children may carry it from both my side and their dad’s family.
I know the feeling being a father myself. I wonder about my kids as well. My recent ancestry is littered with autoimmune diseases on both my father and mother’s sides. Fortunately though there is no history of them on my wife’s side.
Genetics is only part of the story, I’ve seen examples in the literature of identical twins where one twin had an autoimmune disease and the other didn’t. That’s strong evidence of these not being strictly genetic.
So interesting you guys. I wish there were a large study about how many of us had the trigger exposures that have been theorized. I have the family history and I’ve had most of the ones I read about – hair color, heavy cig. smoke exposure, and a certain type of yard chemical… Yet the only thing that I could tie to flares or to the unrelenting RA I have now… is childbirth. Childbirth is a common trigger for some reason & I wonder if this is it. Or could there be more to find? I disagree w/those who say this is a waste of time since like ya’ll I’d do anything to keep my kids from getting this.
Interesting. My grandmother, my mother, my sister and I all have RA. We even have the same quirks of vasculitis and raynolds. Pretty good argument that we are genetically predisposed to the disease. That said, none of us exhibited symptoms until after we had children and more specifically children who at a young age exhibited symptoms of autoimmune disorders. Siblings who did not have children also do not have RA in our clan. Makes me go hmmm
Yours is a fascinating family to study. It would be great if someone would be interested enough to pay for the dna analysis.
Well technology is on your side if you could find someone to do this and study it. I remember the race to sequence the human genome back when I was in grad school and first started in the pharma industry in the late 90’s. It was a tremendous task and it required a lot of labor, time and money (hundreds of millions to billions). The draft of the genome was released in 2000 and called “complete” in 2003. Since then, in 7 short years, the technology has advanced to the point now, with the use of next generation sequencing, you can get your own entire genome sequenced for a few thousand dollars and get the results back in a couple months. It’s truly amazing.
I found this article on a genome wide linkage study on siblings with RA.
http://onlinelibrary.wiley.com/doi/10.1002/art.10147/full
Interesting enough it showed that they confirmed linkage on the HLA region (the one that produces the shared epitope) of the genome as well as a few other loci.
Thanks for sharing the article. Next time I’m in to the rheumatologist I’ll ask if there are any studies she’s aware of. The practice is located at a research university hospital so there is no harm in asking.