Weight of Patient Reported Outcome Measures on Diagnosis & Treatment of RA
Rheumatoid Arthritis Is the Only Major Disease in Which the Patient Largely Informs the Doctor
A funny thing happened while we were at a poster session last week at ACR. The Georgia World Congress Center is like three 4-story shopping malls with a couple of theaters and secondary schools thrown in – it’s big. So, we were standing in one of the several exhibit halls looking at posters of abstracts and listening to the researchers discuss their projects. I heard a man say, “With all of these diseases, you go to your doctor to find out how you are. But RA is the only one of the serious diseases where the patient goes to the doctor for the doctor to find out how the patient is.”
Well if you know me, I was pulled in that direction like an electromagnet would grab a screwdriver. But something stopped me. It was Katie Beth, wanting to point out a poster she’d been reading. Here’s what she wanted to show me: Rheumatoid Arthritis (RA) Is the Only One of 8 Diseases for Which a Patient History and Physical Examination (Versus Laboratory Tests and Ancillary Studies) Were Rated as Most Important for Clinical Decisions by >50% in a Physician Survey. Of course it was the same one. Of course it was Dr. Ted Pincus standing there.
Doctors rate patient reported outcome measures highest with RA
Dr. Pincus was part of a team of five researchers (L. McCollum, S. Park, T. Sokka, H. Yazici, T. Pincus ) who surveyed about 600 doctors (half rheumatologists) “concerning the relative importance of 5 sources of information in the clinical encounter—vital signs, patient history, physical examination, laboratory tests, and ancillary studies—in diagnosis and management of 8 chronic diseases: congestive heart failure (CHF), diabetes mellitus, hypercholesterolemia (HC), hypertension (HTN), lymphoma, pulmonary fibrosis (PF), rheumatoid arthritis (RA), and ulcerative colitis (UC).” As I heard Dr. Pincus explaining, “RA was the only disease for which history and physical examination were rated as most important by >50%, including rheumatologists and non-rheumatologists.”
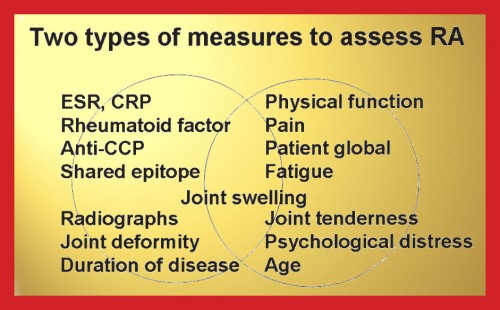
Patient reported outcome measures are more significant than lab tests
 Look at their conclusion: “A patient history and physical examination are estimated by physicians to provide a larger proportion of the information for clinical decisions in diagnosis and management of RA than for 7 other chronic diseases. The patient history and physical examination may be regarded as ‘clinician intensive,’ compared to vital signs, laboratory tests, and ancillary studies. This greater physician effort might be recognized in policies for scheduling, reimbursement, and allocation of physician resources by planners, regulators, and payers.”
Look at their conclusion: “A patient history and physical examination are estimated by physicians to provide a larger proportion of the information for clinical decisions in diagnosis and management of RA than for 7 other chronic diseases. The patient history and physical examination may be regarded as ‘clinician intensive,’ compared to vital signs, laboratory tests, and ancillary studies. This greater physician effort might be recognized in policies for scheduling, reimbursement, and allocation of physician resources by planners, regulators, and payers.”
Imagine: the patients’ physical condition and the patients’ story are more significant with RA than the patient’s lab work or x-rays. Can you see a reason why I say Pincus’ work is important to patients – and doctors? You’ve probably heard me quote Dr. Pincus’ study showing that patient questionnaire scores are as “scientific” as lab tests. In that work, he demonstrated that patient outcome measures are the better predictor of prognosis (via mortality) with RA. He convincingly challenges the rheumatologists who view patient questionnaires as “poor surrogates” of so-called “objective” tests.
Note: You can read this study yourself on page S34 of the abstract pdf at this link. It is number 84.




Pingback: Tweets that mention Weight of Patient Reported Outcome Measures on Diagnosis & Treatment of RA | RA Education | Rheumatoid Arthritis Warrior -- Topsy.com
Great post Kelly. I think that this should really be a wake up call to all of us to be sure to take a more active role in our medical care and to be better in our communication with our rheumatologists.
Thank you. Wake up call to all – doctors who don’t think they need to listen. Insurance who doesn’t realize how difficult rheumatology is. Patients that we’ll need to find ways to be sure our info is correct in our charts (or get new docs). I do have some ideas – there are great tools developed by Dr Pincus that can be used to get this needed patient input in 3 minutes or less I think. And patients could do this weekly online even to regularly track that data – it’s not set up that way now w/ most rheums, but it could be. Most patients I know tell the docs many things that do not end up in the charts. But if patients had direct guided input into their charts, that problem would be addressed. Lots of solutions…
Great points Kelly. A wake up call to all. We all need to play our part, but we should also have the courage, assertiveness, and persistence to make sure that others play their part when they’re not adequately fulfilling their role.
You know what would be really a great thing…For the next ACR meeting to have a panel discussion that includes a patient, a doctor, a payer, a researcher, etc. to share all of their respective viewpoints and problems with the current system. Let everyone involved in the system of patient care with RA see how it all operates and expose the good and the bad. Perhaps something like this could be a catalyst for meaningful change.
That sounds good. Why don’t you write them a letter with suggestions? They are definitely hearing suggestions from me. 😉
That’s amazing information. It’s so hard, though, for me to be super open with my DR or the nurse who checks me in because of the bad experiences I’ve had where I basically get shot down. I will try to be more open. I don’t get a survey to fill out when I got to my Rheum now, but I have the pain journal I created, so hopefully she can use that for help.
Thanks, as always, for posting.
Katie, please see the reply I just gave to RaRAP. It’s not your fault of course, but still our responsibiltiy to try to find a way. In my opinion, as a fellow patient, if your doc continues to get it wrong, you might need to find another one. I’m finding ePatient Dave’s book very helpful. And Elizabeth Cohen’s The Empowered Patient also.
Nice! Someday soon we may be able to fight the disease instead of the doctor.
So well said, Rachel. Your comments are a blessing always.
There is an excruciatingly fine line between many doctors’ perception of a patient as involved & educated versus obsessed and hypochondriacal. Hopefully, as doctors like Pincus speak out, that line will move in favor of patient participation. Thanks for another excellent post, Kelly.
Great point, Jackie. I have found that this depends upon the doctor’s personality. The doctor really has the responsibilty to be getting this information from you. There are great tools for this that Dr. Pincus has developed. It only takes a couple of minutes to make a valuable assessment of RA activity w/ these tools such as RAPID3. The onus is on the docs here.
I do journal my pain, and have found one of the best disease journals is my digital camera! I have shot before and during photos of my misbehaving joints, and have organized them on my laptop by joint. The photos are automatically dated and timed, and I bring my laptop with me to rheumey visits…a picture is worth a thousand words, especially when I go for an office visit and am having a good day.
Goodmorning Kelly..and friends…Im gearing up for my visit to my Rheumy and im nervous! Im going to ask her for the doctors notes and labs..She is not going to like this at all! Im trying to memorize my questions because she doesnt like to see a List. Why do i have to be afraid? Its about me not her. I read about all of you and your relationship with your doctors and i wish i could have one like that..Well back to studying..Thanks for going to ACR..Its very interesting what u have learned..Judi
Dear Judy,
I’ve had so many appointments like that. Even now with the great doc I have, I worry that I’ll do something to make the doc mad because I feel afraid to lose the good doc it took so long to find! The medical assistant is gruff with everyone & I worry that she’ll say something untrue & the doc will blame me… Anyway, I understand feeling intimidated! It’s just the nature of the relationship in some ways. I’m reading Elizabeth Cohen’s book The Empowered Patient that explains a lot about why it’s like this. Try to think of us being there with you. It has been helping me to think that way.
This could not be more timely. I had to see my regular physician who follows me every 6 months for high blood pressure, etc. I was in the throes of an intractable RA flare so he had me get labs done. Of course, my labs were beautiful as they always are (except for elevated ALT and Calcium) so no “flare” was indicated. However, I was at my rheum’s office one day later and was prescribed Medrol dose pack. As much as steroids can be feared, it is the ONLY thing that quells my flares. My pain and stiffness in my fingers, shoulders, ankles, etc. were eased and ameliorated after a couple days of taking the methylprednisolone. How very wonderful that my doctor’s office believes me when I describe the pain and the way it affects me. I may need to stay on low-dose prednisone to keep this beast at bay. But I think it’s worth it.
Good points, Ruthe. I’m glad your rheum doc pays attention to signs of disease activity besides blood work.
I think you could say that about all the autoimmune diseases. My doctor talks to me in length about how I am feeling and what is new. I have routine labwork done,but we talk mostly just about me and how I’ve been doing. I was diagnosed with Lupus 25 Yrs. ago, and just recently with RA.
Im not as educated as should be in the study of RA.Only several years ago ”I being a white male 50 yrs old at the time” was given lab work by my family doctor and it came back great.He said get on outta here you have a little inflamation in your blood but then who dont.It went the next several years in pain ,swelling ,and deformity.Each time i would say something to the GP it was the same ”your labs are fine go home” with a slapm on the shoulder.Finally my wife loaded me up and took me to the joint Dr…..I got into his office and he comes in and says how long have you had RA? He said your hands and feet show classic signs of RA.I told him about my journey with my regular Dr.and he said ”happens all the time”So blood test is a valuble tool so is common sense.
Indeed!