Aftermath of the FDA Vote on Pfizer’s RA JAK Inhibitor, Tofacitinib
After the tofacitinib FDA hearing, the votes are in, false perceptions persist, and patients still need relief.
Some estimate that tofacitinib could be approved by the US FDA within a few months after mixed votes and mostly inaccurate press reports. It’s fitting this discussion takes place as rawarrior.com begins its fourth year of reporting the patient point of view Thursday. Many are hopeful for a new treatment and never was the patient perspective more essential!
The PANEL: 4 distinct votes about approval of tofacitinib
The FDA Arthritis Advisory Committee (AAC) actually took four votes on tofacitinib at the end of the meeting May 9th. They voted 2-8 on the first question, finding that Pfizer has not sufficiently demonstrated that tofacitinib stops radiographic damage. Pfizer hopes forthcoming clinical trial results will address this concern, according to one source. The second vote was unanimously in favor of Pfizer, that the clinical trial data provide substantial evidence of the efficacy of tofacitinib for the treatment of moderately to severely active Rheumatoid Arthritis. Another vote, with regard to the JAK’s safety profile, was split: 7, yes; 2, no; 1, abstain. Finally, 8 of 10 recommended approval for use after failure of one or more DMARDs.
One of the two dissenting voters, Dr. Sharon Gabriel of Mayo Clinic, explained that she would support the application if the language were more restrictive so that an RA patient might not move directly from failing a weaker DMARD such as Plaquenil directly to the new JAK inhibitor. With the long track record of methotrexate, Gabriel’s point is valid. The wording will likely be modified so that patients will have to try more than one disease modifying drug before getting access to tofacitinib.
Although Pfizer’s tofacitinib application will likely be approved, it may not be approved as a first-line DMARD yet, but either a second or third-line drug. When approved, Orencia and Actemra were used similarly; patients had to have insufficient relief from DMARDs and TNF inhibitors.
Access the entire New Drug Application (NDA) briefing document (254 pages) “Tofacitinib for the Treatment of Rheumatoid Arthritis.”
The PRESS misses the mark because they have no idea
We watched a variety of TV reports Wednesday evening to see how the tofacitinib hearing was handled. We’ve also read a few news articles over the last few days. Clearly, most of the press know as little about Rheumatoid disease as the rest of the public knows; they remain confused about what the disease is or how badly new treatments are needed. None were completely accurate; some are funny even if they’re sad.
Pretty good: Medpage Today has a good article about various points considered by the AAC as they debated and voted on the NDA for tofacitinib.
The bad: The Wall Street Journal gave the following as their entire explanation of RA: “Rheumatoid arthritis is a chronic inflammatory disorder that usually affects small joints in the hands and feet.” Wouldn’t it be nice if Jennifer Dooren were correct, but alas, she’s not. One wonders whether she did her research by reading Woman’s Day magazine.
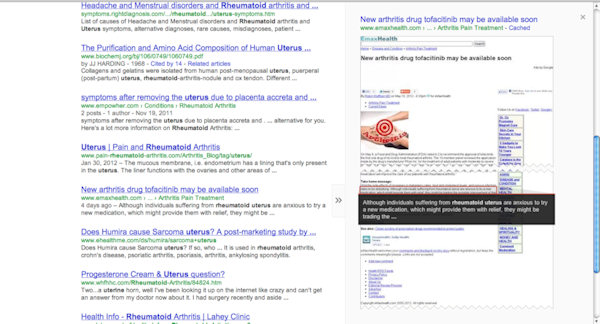
The ugly: An article on EmaxHealth takes the cake. “Although individuals suffering from rheumatoid uterus (serious proofreading error – yikes!) are anxious to try a new medication, which might provide them with relief, they might be trading the possible improvement of their arthritis with another, possibly serious problem… Arthritis sufferers who have not tried aspirin should discuss its use with a healthcare professional, ideally a rheumatologist.”
Does anyone believe the press would recommend aspirin (or Tylenol) as a treatment for Lupus, MS, or Lymphoma? This happens to RA patients because the disease is misnamed Rheumatoid Arthritis. We know that RA is not a type of arthritis, but that arthritis is only one symptom of a serious disease that can affect vital organs; but these reporters apparently do not.
The PATIENTS, the principal stakeholder, have no vote, no press agent
Patients are the reason for the decade plus of research leading to tofacitinib. Patients are the biggest stakeholder in this decision and the only ones with a full appreciation of what the disease entails. We are not “anxious to try a new medication;” rather, we deserve effective treatments that will stop disability and premature death as much as victims of any other diseases do.
Edit: Wall Street Journal article link updated after WSJ deleted the page. New link shows same article from May 9 2012 still appearing on other sites.
Recommended reading
- Video Blog: Two Essentials with a Rheumatoid Arthritis Diagnosis
- Keeper or Loser: I’m Not Giving Up, But What Do You Think?
- 6 Ways to Get Hard Projects Done With Rheumatoid Arthritis
Postblog: Victim is a word seldom if ever used on this blog; however, it seemed to fit this context best.
EDIT 5/15/12 2pm ET: After several negative comments on his site, prompted no doubt by this posting, the author of the emaxhealth article has edited his page so that it no longer reads “rheumatoid uterus.” However, the obgyn doc stands by his erroneous statements about RA treatment. Unfortunately, our community’s attention to their site is likely benefitting them financially. Below is a screenshot from Google, showing the rheumatoid uterus quote.
I hope the inadequate way the Wall Street Journal defined RA will not be lost in this discussion. This is far more grievous given the trust readers have in their publication and the size of their readership.




How are we suppose to ever get help when this is the latest nursing continuing education:
http://www.medscape.org/viewarticle/762231?src=cmemp
From Medscape Education Clinical Briefs
New Evidence-Based Treatment Recommendations for Inflammatory Arthritis CME/CE
News Author: Janis C. Kelly
CME Author: Hien T. Nghiem, MD
Faculty and Disclosures
CME/CE Released: 04/18/2012; Reviewed and Renewed: 05/02/2012; Valid for credit through 04/18/2013
The recommendations include:
• routine measurement of pain using the visual analog scale, numeric rating scale, or verbal rating scale;
• paracetamol (acetaminophen) as the first step in treatment of persistent pain;
• avoidance of systemic glucocorticoids for routine pain management unless there is also inflammation;
• tricyclic antidepressants (TCAs) and neuromodulators for adjuvant use only, and no use of muscle relaxants or benzodiazepines for pain relief;
• adding a drug with a different mode of action if acetaminophen or nonsteroidal anti-inflammatory drug [NSAID] monotherapy is inadequate, but not combining 2 or more NSAIDs;
• using the lowest effective NSAID dose;
• attention to existing guidelines for the safety of specific drugs during preconception, pregnancy, and lactation;
• methotrexate can be safely combined with standard doses of paracetamol and/or NSAIDs (excluding anti-inflammatory doses of aspirin, >650 mg/day);
• acetaminophen as first choice for pain relief in patients with gastrointestinal comorbidities, but only cautious use of non-selective NSAIDs in combination with proton-pump inhibitors (PPIs) or COX-2 selective inhibitors with PPIs; and
• acetaminophen as first choice for pain relief in patients with preexisting hypertension, or cardiovascular or renal disease, and only cautious use of NSAIDs, including COX-2 selective inhibitors.
“Important questions that remain include the extent to which our patients with IA require regular analgesic medications in the current era of aggressive (and generally successful) control of inflammation (interestingly, the scant existing data suggests that the use of NSAIDs and opioid analgesics has not declined in the last decade, and may even have increased), and the role of novel pain-modulating drugs in this population (such as the gabapentinoids). Well-designed prospective trials of analgesic drugs, either alone, in combination, or in series, are clearly required in this population.”
Hi Tanya. Thank you for pointing this out. There was a recent publication recommending acetaminophen in rheumatology / RA patients. I supppose that prompted this. I’ll look around for it – I remember debating about it on Twitter with someone – it seemed foolish to me to recommend such high doses of Tylenol at the same time its liver dangers have become apparent – and to patients who will be needing it DAILY over a period of DECADES and are taking other things which give the liver extra work to do [95% of RA patients are prescribed methotrexate & a majority are on a cocktail of drugs for various RA symptoms & comorbidities]. And then there’s the fact that acet. doesn’t reduce inflammation & seldom adequately addresses pain even in headaches, much less RA, which is 100 times worse than an average headache…
Indeed the tylenol piece is infuriating, however, what can we expect when the doctors hold the belief that:
“Important questions that remain include the extent to which our patients with IA require regular analgesic medications in the current era of aggressive (and generally successful) control of inflammation
shame on me for missing that quote – that’s the kind of thing I find and shine a spotlight on so patients will *know* why it is their doctors think it’s all in their heads… Thank you Tanya. I know that belief is out there – that’s why some docs measure crp & tell patients that they are in remission based on “inflammation markers” despite continuing symptoms… This, my friend, is our battle. With God’s help, one day this view of not treating pain because of false notions about blood tests will be seen as barbaric as we patients already know it is.
Finally found those multi-national tylenol recommendations I had read last month. Here: http://rheumatology.oxfordjournals.org/content/early/2012/03/23/rheumatology.kes032.full
As a patient, they do not sound compassionate. As a person who has read a lot of research & recommendations, elevating tylenol’s role in this way sounds like a huge step backward in rheum care.
Gosh Tanya, thats as bad as the “take an asprin and call me in the morning…” After reading Kelly’s recap of the “media” reports, I didn’t think my jaw could drop much further…it just did. What is WRONG with these people? Why are “funny named” diseases taken seriously and RA (D) is NOT? I just don’t get it! Maybe we need a million patient march on DC (more like roll in wheelchairs) and we can dump a pile of tylenol and asprin on the mall! And what is the connection with Tylenol and the medical world? Its always the first thing they tell you to take, but it really doesn’t do much….no inflammation reduction and it ruins livers! The Tylenol folks must have some hold on someone that they continue to use that as pain reliever #1….I’m gonna be growling all day now…..
Good morning Nancy. I wish I knew why…
My readers know I don’t subscribe to conspiracy theories, but this is certainly odd. It would be very difficult for Tylenol to be approved today, with it’s side effects & risk – benefit ratio. In many patients, it’s shown that a large percentage of the drug ends up in the liver & doesn’t even make it to the tissues (pain site). How could anyone logically recommend it for patients with severe pain in numerous locations as RA usually brings. It makes you wonder what is influencing these reports. Something beyond the science.
Keep in mind that many in the medical profession subscribe to the myth that RA pain is not very bad, but has been exaggerated for centuries by the patients who claim that it is severe… there are a number of posts here on that topic – here is a list of some: https://www.rawarrior.com/tag/pain_tolerance/page/2/
Do you think that could be part of the reason?
Again the press does a great dis-service to us as sufferers from RA. But the press response is based on what they see everyday. And unfortunately they do not see the results of what is truly severe rheumatoid disease. They do not see the heart complications or the complications when it attacks your cervical spine. That is where we come in and must make our voice heard. “Have I talked to my rheumatologist about taking asprin?” You must be joking.
oh yea, David – – didn’t you know aspirin is the latest in RA treatments. Why else would Pfizer spend a billion to develop a JAK drug? 😛
As I was reading about how the votes went on this new drug I was not surprised at how the press reported it, that’s par for the course but not right. When I read that just try an asprin I think steam came from my ears. That is like telling someone with a heart blockage to try asprin before we open the blockage. I take asprin everyday but my RAD is progressing. Makes me realize even more the name needs to change.
well said Sharon & David.
Thanks Kelly for this recap.
I just left a comment on the emax website.
This was perhaps the most infuriating and ridiculous piece I’ve seen lately. Aspirin as a comparable treatment to a DMARD or biologic? And this was supposedly written by an MD? That is the saddest part. I’ve seen first hand the efficacy of aspirin for RA, PsA and AS, as various elder members of my family were told to take it to treat these diseases. Multiple joint replacements, a fused spine and several heart surgeries later, it became apparent that aspirin couldn’t begin to fight these aggressive beasts. It is like saying that you could kill an elephant with a pellet gun (not that I would approve of this, but I needed an analogy).
Ugh, I agree on the aspirin thing. When I was dx with JRA in 1982 I was put in aspirin therapy. That was pretty much it then (mtx and gold were reserved for extreme cases, and dr’s didn’t want to use them). I can first hand say that taking handfuls of aspirin for years didn’t do much of anything for pain, and only helped moderately with the inflammation, while making me bruise and bleed and wrecking my stomach so I could hardly eat. I’ll take the biologics ANY DAY over aspirin therapy.
Of course! And who would think of recommending that patients do not receive disease treatment? No one with any knowledge of the disease at all.
Thank you Kelly for keeping us all in the loop. Until all of these policymakers can feel our pain or see someone they love go through or walk/hobble a mile in our shoes they will cannot make intelligent decisions. Is anyone besides all of us paying attention or listening? Thanks for being our voice.
Really really really sorry to post this question here, because it’s not at all pertinent, but can anybody point me to a place to ask about finding a good rheumy? Very discouraged after my last appt, not being listened to, taken seriously. Would like to find a better one. Again, please just point me in the right direction. I’m very sorry to butt in. Really irritating to continue to see people having no idea what RA is, especially when all my rheumy says is take 1800mg ibuprofen a day, and folks at church (who genuinely care, however) can only think of miracle diet cures. Whom do we petition to get the name changed?
Hi Tom – I am leading the charge about the name change – so you came to the right place. Please subscribe at teh top of the page & stay tuned for more info on that – when the site opens for membership – VERY soon at rheum4us.org, you can join. And sign up for the newsletter there too & we’ll keep you informed on how to help.
We’ll eventually have a recommended dr list for members there – but right now, you can start by looking over the comments on these 2 posts: here: https://www.rawarrior.com/santa-bring-her-a-rheumatologist-please/ and here – https://www.rawarrior.com/the-appointment-with-doctor-perv/. If you don’t find someone good that way – you might ask on our Facebook page – the best way to find a decent one is by word of mouth from another patient. I do NOT for the LIFE of me know how we have so many like you describe, but I do agree it is not to be tolerated if things are to change. That is the only way change will come: we move away from dismissive docs who don’t take us seriously and toward those who want to treat us instead of argue with us. I’m sorry you were treated that way, but please know you aren’t alone – we hear it all the time.
Thank you so much for the reply. Looks like one rheumy is near me who has been mentioned in the article you linked to, whom I may contact. There is one also in Exeter, NH, which is only just over an hour from me, and I may stop in some day soon. I simply cannot believe I’m supposed to sit around and take ibuprofen and that’s that. Pain is a symptom, a sign of something bad going on. Do I have to wait until I’m crippled before a doctor will take me seriously? If that’s the Lord’s will, I will follow, but it doesn’t seem right. Anyway, thank you so much for your response, and congrats on four years.
You are completely right in what you say about symptoms & treatment. It is so sad to hear from people almost every day who go thru this battle just to be treated. Don’t give up; you aren’t the only one. And no, I don’t think the Lord wants us to sit back & just let nature take it’s course – I think he gives us science & doctors & other people with compassion so we can fight the disease. Although I understand accepting what we cannot change – that’s not surrender. Just my view.
Two days ago, I watched a thirty-something neighbor exit her front door and creep, bent over, down the sidewalk toward her parked car. Her face was drawn, whether from pain or from the approximately thirty pounds she has lost without trying over the last few months. When she opened the door of her mini SUV, she had trouble getting into the car, but I couldn’t walk fast enough to get to her and wouldn’t have been able to help if I had because walking is an activity I’ve just begun to take up again after a year in which walking a few steps was difficult. I knew that she had recently been tested for RAD, and I personally didn’t have to see the results to know the answer. She walked and looked like I did a year ago, while also waiting for my diagnosis. I learned later that day that her disease had, indeed, been confirmed, but I knew already. It’s about way more than small bones in the hands and feet.
Indeed, the old saying, “takes one to know one” – I do recognize it when I see it too. I’m glad you’re able to walk better now and it will certainly be a big encouragement to her to have you to talk to! It is shameful that the Wall Street Journal would say that.
I came across this article and thought it was interesting concerning when health insurance will pay for this drug upon approval.
“Reimbursement Intelligence: Tofacitinib to Be Positioned After Anti-TNFs, Say Payers Based on FDA Panel Review”
http://www.marketwatch.com/story/reimbursement-intelligence-tofacitinib-to-be-positioned-after-anti-tnfs-say-payers-based-on-fda-panel-review-2012-05-15
Yes, I saw that too & hesitated to post yet another article on Tofa, but I do think it warrants discussion for several reasons. Thanks for posting Tonisa.
Lost in the discussion is the fact that tofa is an ORAL pharmaceutical, rather than the normal injectable biologic, which would be a big deal to those having an aversion to needles (like me). Does the patient have a say? I would want tofa as a first line therapy.
Good point. No, at this point not – we have no voice on the committee – I doubt it will be a first-line tx unless Pfizer can come up w/ some great numbers both on safety & x-ray progression.
Hi Kelly
Someone mentioned the need for a Press Agent to help get the patients’ points of view accept in the press. May I suggest that this is something that the Foundation might follow up. Getting a recognised agency to handle the foundation’s account would be a great step forward.
I guess it would be expensive, but perhaps {???} one agency might take it on as a ‘charity’ or ‘public service’ activity. And if it was an agency that employed someone with RAD or with RAD in the family, we would get even better coverage.
Just a thought. Keep up the good work. [hugs]
Barbara
We are working on this 😉
Also just noticed an advertisement on this page [I know it’s NOT your choice what turns up there].
Just above the text “What do you think?’ is a small box, thus—-
Arthritis Pain Relief
Instant Relief from Acute and Chronic Arthritis. Get proof with Free Demo at ArthriticPainRelief.com.au/FreeDemo
shall have to investigate!!
Barbara
Kelly, we have you! That’s not too shabby!
All my rheumatologists have very forcefully voiced their opinion not to use Tylenol-like OTCs for additional pain relief above my prescribed pain killers. I believe Aleve is the one that gets the okay the most. When did rheumatoid arthritis change to be called inflammatory arthritis? Is this article even ABOUT rheumatoid arthritis, but maybe osteoarthritis? Very confused here about the verbiage used as I don’t see the words “rheumatoid arthritis” anywhere. Very discouraging. I vote for the 1,000,000 RA Roll on DC.
Hi Cathy,
Inflammatory arthritis (IA) is a category and RA is the largest segment of IA. Other diseases that are IA include Psoriatic arthritis or Lupus.
OA is not inflammatory, although a minority of drs have recently begun to use the phrase “inflammatory oa” which really muddies the water. Some people diagnosed w/ “inflammatory oa” are eventually diagnosed w/ RA by a second opinion. I hope that helps your confusion a bit.
and yes, most good drs & pharmacists would agree w/yours. People with chronic painful inflammatatory diseases are usually not treated by tylenol for several reasons.
And why exactly is an OBGYN writing an article on this anyway??? When people who have no experience or knowledge of a disease attempt to write an article, their uninformed drivel is exactly what makes it so hard to get the truth to the public. It would be like me writing an article on pediatric nephrology. Writing an article for the sake of writing an article is of no benefit to anyone. Absolutely ridiculous!
yes, and while he was just re-hashing what happened in the first part of his story, it was not a problem. But then he wrote “take aways” and gave what sounded like medical advice. Bad medical advice. I did not comment there, but rather filed a complaint to the HONcode when I saw their link in his footer, because of bad information that could hurt patients, presented from an MD, who is not even a specialist in rheumatology.
I left comments for both the emax and WSJ articles. How infuriating!
I’m horrified by that statement in the highly-respected Wall Street Journal. Unfortunately, I would have had to sign up for a trial subscription in order to read the whole article, and I certainly didn’t want to give them that support.
We should all write to the WSJ in every way we can–Twitter, Facebook, email, good old fashioned snail mail. This is an egregious error that has no place in a trusted and distinguished newspaper.l
Thanks. Their Twitter is @WSJ. I’m sure they’re easy to find on Facebook.
I think that an OB/GYN has no right to speak as an authority on Rheumatoid Disease. I wouldn’t want my rheumy to deliver my baby, even though she is a great doctor. They specialize for a reason. I believe we will never get the help we need because there are too many of us. If we are characterized as disabled, we would be entitled to some help through are government. The climate we have now in government is not a helpful one. There will be no plans to expand benefits to us. No more money will be spent looking for a cure. If the media continues to portray us as simply patients with a little soreness, no one will help. And we all know who owns the media. It’s no accident that the Wall Street Journal portrayed us this way. This a very conservative paper. The far right feels we are all whiners. Find a corner and shut up. That’s their motto. If this problem isn’t addressed first, nothing will change. How do we change the attitude of half of the US?
Pingback: A Time To Laugh | Bringing Me Back Home
Pingback: Rheumatoid Chaos! « Ancient Reptile
Hi Kelly, I just discovered your blog and I’am so thrilled to find a community of RA patients like myself. I’am very interested in this new drug, Tofacitinib.I have tried to research the ingredients and can not find any site that publishes them. I’am highly allergic to Polysorbate 80(also called Tween)They put this in a majority of RA drugs. Would you happen to know if this drug has that component? I’am currently limping along on Orencia, which is only partially working for me. I have a life threatening allery to all Non-steroidal antiinflammatorys, so of course I am also on Prednisone.Hoping this new drug is the one for me. Thanks,Ann
Hi Ann. Welcome! I hope youre still reading – I’m catching up on comments today. Since polysorbate 80 is an emulsifier and the tofa med will be a pill, I’d doubt it. But that will info may not be available until the compound is approved and the insert is published. After that, you could contact Pfizer if you can’t find it in the insert.
Dearest Kelly,
Your doing a terrific job at spreading RA awareness and I’m very proud of you for doing that. My name is Amy and I to Doctor at the Mayo Clinic in MN. I came up with a plan and ran it by my Reumatogest Dr Matteson. And we both thought it was a wonderful plan but we need to get it goin. I only want to tell you about this over the phone and I will need you as a speaker. Let me tell you a little about myself. 12 years ago I woke up with the worst pain in my right arm and couldn’t move it. I was in tears so I woke up my husband and he put me in the shower with hot water. That barely helped so he called the ER and they suggested ibruprufin and Tylnol be switched every 4 hours until I saw my Dr. Well my white blood count was so high she made an appt for me to go to Fargo. There I was told I had RA! I didn’t even know what it was lolol!!!! I talked to my Mom and were originaly from southeren MN around Rochester. So my local Dr in Fergus Falls MN (Vacation Country) got me in. And you know how it is your there for about 5 days and they find out everything that is wrong with you lol! I also found out I suffered from 2 more arthritis and many other diseases UGH! Then I met my HERO Dr Matteson! He never sugar coated anything and last spring even told me I was one of his miracle patients and should of died years ago. Now I suffer from 5 arthritis and have turned it all into a positive. RA is now in my liver and Ill need a liver transplant down the road. BUT while Im on this BEAUTIFUL world that God has given us.
NOTE: I have deleted Amy’s personal address and phone number and will contact her directly. ~Kelly
Amy, I will email you directly. I have saved your contact information.
A couple of years ago patients in this community created the Rheumatoid Patient Foundation to directly serve those with this disease. We would love to have you working with us and I’ll be glad to talk with you on the phone soon. Meanwhile, please visit the RPF site also here: http://rheum4us.org.