An Unremarkable Reality: Scans Don’t Lie – or Do They?
Show me your erosions or else
 Some of you may remember last year when we met Dr. Shrug who gave my foot an ultimatum: Show me a bone erosion, or no more DMARDs. We only ever saw the doc once (more than enough). It was Dr. Tylenol’s partner, who they scheduled us with since Dr. T was out.
Some of you may remember last year when we met Dr. Shrug who gave my foot an ultimatum: Show me a bone erosion, or no more DMARDs. We only ever saw the doc once (more than enough). It was Dr. Tylenol’s partner, who they scheduled us with since Dr. T was out.
We saw the report from the MRI. It said my foot was unremarkable. That foot does not have my worst affected joints, but they are obviously affected. I knew the MRI was wrong, but I was helpless to object: I called the imaging center to be sure it had been read properly, and not mixed up with someone else’s scan. End of story.
A few months later, I was copying records for the physical medicine doctor that my GP sent me to… and what I did I happen upon? Old foot x-rays notating joint space narrowing and early erosion.
I don’t read MRI’s for a living, so I can’t tell you whether the MRI itself or the radiologist was in error. But I can tell you that my feet – and the rest of my body – are affected by Rheumatoid Disease (RD), so that the past eight years of my life are entirely different from what came before. Whether or not any particular MRI identifies that.
Remarkable realization about radiology
 Of course deep down I knew the MRI report had to be wrong, but there was nothing I could say. They stood by it and I didn’t want to pay for a new scan. If you do a little digging, you can find that radiology is an art, machines differ, and mistakes are common (such as in the x-ray story below).
Of course deep down I knew the MRI report had to be wrong, but there was nothing I could say. They stood by it and I didn’t want to pay for a new scan. If you do a little digging, you can find that radiology is an art, machines differ, and mistakes are common (such as in the x-ray story below).
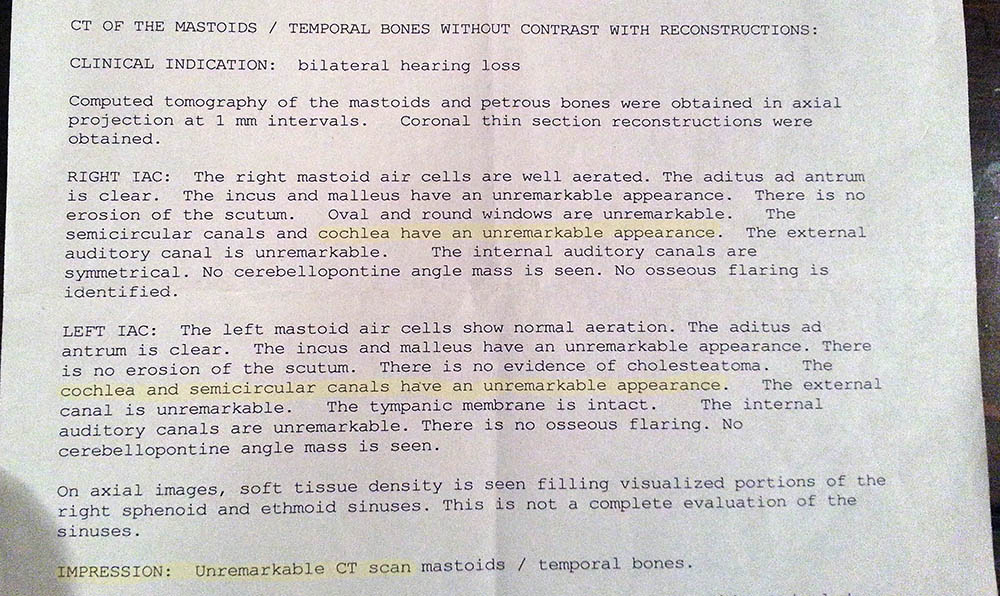
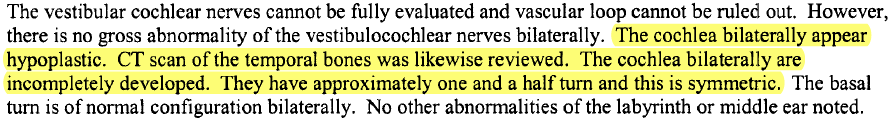
Last week, I was collecting my son DJ’s records related to his Mondini diagnosis and I had to pick up a disc of a CT scan at another imaging facility. It came with a report. I brought the disc and the report to Roo’s doctor and never thought to look at the report – I knew what was in it – his cochlea only has 1.5 turns instead of 2.5… old news. But then I slid the paper out from the disc jacket and read: “cochlea have an unremarkable appearance.”
I’d already read the other specialist’s evaluation “The cochlea bilaterally appear hypoplastic… The cochlea bilaterally are incompletely developed. They have approximately one and a half turn and this is symmetric.” That is one of the three features of classic Mondini.
The local doctor had misinterpreted the scans. The other specialist who evaluated them had commented to me about the poor quality of the scans, and I remember being surprised that MRIs and CT scans (we had both) could be done poorly. They tell me the magnets are various sizes and machines have to be calibrated, but that’s all I know. Maybe a radiologist or radiology technologist would like to comment.

What can clinicians take away from this story?
1) Test results may be informative, but can also be subject to error.
2) Don’t dismiss a patient’s symptoms based on a test. Treat the patient, not the test.
What can patients take away from this story?
1) Imaging is very expensive unfortunately, so it’s not likely that people can get scans repeated easily. However, if you doubt the results of any scan, ask your doctor to request it be re-read. If you have a supportive doctor, that would be a good first step.
2) Save your old reports so that you can compare them to new ones. This is also true for lab reports. When one lab said I had a zero anti-CCP level, my GP and I both new it was an error since I had a half a dozen noting “>250.”
Related stories
We’re not the only ones who’ve met a Dr. Shrug. It’s so important that you don’t give up. I clung to that after Sara commented “My doctor shrugged it off after the blood test. If the pain in my hands wasn’t so debilitating then…” Continue reading… Don’t Give Up
It’s an important lesson – don’t let the x-rays fool you. A few years ago, we helped a friend after a terrible fall. “None of the doctors doubted the x-ray machine or x-ray technician or the doctor who read the x-rays. I am afraid that the only one who was doubted was my…” Continue reading… Hysterical Symptom Diagnosis, Part 1




Yes! Been there and done this. Kim has had terrible foot pain for years now. She had X-rays done and they came back as normal. Then the fourth and fifth toes on both feet started rotating over. Her fifth toes are rotated so far you almost can’t see the toenail when looking down on them. She also developed large nodules on top of her feet. Again, the X-ray was “inconclusive”. When we pointed out the bump and toe rotation to her rheumatologist his reply was, “You’re old. People’s feet do that when they Getty old.” Umm. She’s 43. Anyway, took the same six month old X-ray’s to a podiatrist and he looked at them and pointed out the joint erosions in the fourth and fifth toes. He also explained that the nodule is a calcium deposit because her foot is starting to deform. Same scan. One doctor saw nothing, another saw everything.
Thanks for sharing Eric. Sometimes people are lucky on the first shot, many are not. It helps to know they aren’t alone and not to give up.
I hope you got a new Rheumatologist. I dropped mine because she wasn’t helping with my pain and found a great Doctor that I love!
Thanks for this excellent point.
I have had this experience with radiology as well, the worst being a rheumatologist who admitted sitting with the radiologist and telling him in advance what he expected to see on scans, based on labs, and then having the radiologist “read” the scans to support his presuppositions. The results were in direct conflict with previous scans I had done.
Thank you for pointing out the misconception that scans are clear and unequivocal and all abnormalities can be seen without question and in the same way by any reader. It has serious implications, as you yourself found, for patient ability to get further treatment, see further specialists, etc.
An excellent chapter on the subjectivity and art of radiology, and the problems connected with it, written by a physician:
Jerome Groopman, M.D., “How Doctors Think,” New York: Houghton Mifflin, 2008 (chapter 8: “The Eye of the Beholder”).
This is an excellent book overall that many who struggle to be heard by doctors might like to read. Also excellent, his book “The Anatomy of Hope: How People Prevail in the Face of Illness,” 2005.
So true! Back in 2007, after having undiagnosed pain for a couple of years, my primary care doctor actually told me to see a psychiatrist, that she could find nothing physically wrong with me. Then my knee went out and I fell. She said the X-ray and MRI showed nothing — “just a little osteoarthritis.” And that is what the reports say. But I could hardly walk so on my own I found an orthopedic doctor who suggested a torn meniscus. After he did surgery to repair it, he said to me “Why didn’t you tell me you have RA? How long have you had it?” And that is how I got my RA diagnosis! The surgeon found terrible synovial inflammation and damage in the knee. I still have my “nothing remarkable” reports but I longer have that knee because it had to be replaced a few months later.
As a healthcare professional I can say this is definitely true. We read all our own xrays, ultrasounds etc. We get the reports but really don’t pay that much attention to them, because we see these films everyday this is our life long job and we know what to look for. We also know the patient and what is happening with them. A lot of films and studies are over read in our case but it just points out that reading these reports without knowing the patient is difficult.
I am so sick of the runaround from Dr’s.
A friend just told me that her rheumatologist says the lab reports are OK but symptoms are what really counts. Don’t we wish they all got that?
Thanks for posting this, Kelly. I haven’t had any of my scans re-read or re-done for financial reasons, but I wouldn’t be surprised if at least 1 of them were to have a different outcome. Additionally, after having such pain in my hips that I was walking with a limp, my first rheumatologist told me she ordered an MRI of my hips but I was surprised to find out at the follow up that they only imaged the SI joint (only part of 1 hip visible on the scan). Perhaps this is normal practice, but I still think she should’ve at least explained that before the scan happened. I sometimes wonder if my “normal” scan was only that way because she didn’t actually image the hips where my pain had been (and insisted it was referred pain from SI).
And boy, was it hard to find a doctor who would listen to me when every blood test was normal, and scans were unremarkable. I was also walking with a limp, falling asleep at my desk mid-afternoon, and just holding my coffee mug required both hands or I’d drop it from pain/weakness. Thank the Lord for doctors that listen to the patient!
This is another one for the “Believe It Or Not” file. As hung up on imaging as most docs are, you might think there would be some standardization and competency in reading them.
My first set of hand x-rays, about two years ago- actually, I had several sets done the preceding year- the first set done for a rheumatologist showed significant thinning of the bones. She said that proves chronic inflammation, and started treatment. Rheumy #2, Dr. Disaster, took new noes a year later. He said they showed narrowing of the joint spaces throughout both hands (not present the previous year), but “that doesn’t mean anything” and said that the thinning of the bones “is subjective, and we don’t pay attention to that.” Huh??
A couple of years ago one of my kids dropped a microwave oven on his foot. They told him at the ER that it was just a flesh would, 12 stitches worth, but when he went back to get the stitches out the doctor asked what they were doing about the break and showed him a loose piece of bone on the x-rays taken originally.
I have read that since so much imaging is now done autopsies have become rare. “We know what was wrong with him and what he died of.” I wonder.
I have had a lot of MRI imaging in the past year that came up unremarkable. This is despite the fact that my hands get so visibly swollen and red that they look like lobster claws. My case is further complicated by the fact that I am completely seronegative. Fortunately, I found a rheumatologist who explained that because inflammatory arthritis is cyclical and unpredictable, imaging cannot always be scheduled at the exact day or moment necessary to capture abnormalities. I am finally getting treatment, even though on paper I am unremarkable. (I hate that word :P)
Ten years ago I had MRIs of both hands that showed damage. Unfortunately, I was a dumb college kid back then who did’t ask for or keep records.
Lesley, you *can* get those older studies, if you think your doc would be able to make use of them. Write to the institution through which you had them done. They may have to go back in the archives, but they are required to get them for you. They will charge a reasonable fee for copying them. Be sure to ask for copies of the original films, not just the reports.
Reading radiologic films is a craps-shoot. There is so much that is subjective and interpretive about it. For a while there was a movement to have computers read radiographs. In many instances, the computers were even worse than the residents. Now there frequently is a combination approach – computer plus one or more radiologists.
There was a case, years ago, of “missed” lung cancer. The patient had been having chest X-rays yearly for the previous 10 years. When they looked back at the 10 years of studies, with the knowledge that the patient had lung cancer, they “found” the primary, shadowy tumor in the first year’s study. It had been missed each year until the 11th year. The patient died a few months later. And this is not unusual. Even now there are cases of missed tumors – both by machine-read and “people-read” studies.
I’m not trying to excuse the medical professionals who miss things. The system of reading and re-reading radiographs needs to be examined and corrected. No doubt. So, too, the proper radiographic techniques in taking the films.
When we find and tell our physicians about errors, it threatens them, their education, their profession and their standing in that profession. In the 19th century, doctors had no knowledge other than anatomy and a bit of physiology. They gained their reputations by being kind, humble and admitting that they didn’t know. By the mid-to-late 20th century, they had become afraid to admit they didn’t know something. Now, not admitting lack of knowledge has become engrained into the profession.
SIGH! Makes our jobs as patient harder.
I really, really wish training in the medical field included serious time assessing and listening without high tech, diagnostic machinery.
i will never forget being strapped to some machine that was supposed to be monitoring contractions. (I will spare the men the details) i kept trying to get someone, anyone to listen to me that i needed help NOW. May as well have had third baby alone in a corn field. the OB walked in as i was crowning. the MACHINE was still recording “minor” contractions. the nurse is scolding me for not giving her time!!.
guess it is time to get trained in radiology, etc… so we can test and diagnose ourselves.
NVk
I can’t emphasize enough how important it is to get scans and X-rays re-read if you know in your gut something is wrong. Several years ago I was in a bad accident and shattered the talus bone in my ankle. After two surgeries I was still in pain, increasing pain, and something felt terribly wrong. I had a good doctor who was board certified, highly praised etc. After a long few months of me insisting something was wrong and him and the radiologist insisting healing was fine, and the doctor finally suggesting I just having trouble emotionally “processing” the pain I was able to get to another doctor and have the X-ray read again. Diagnosis: avascular necrosis, meaning the bone was dying throughout that bone. I ended up having my leg amputated below the knee. I don’t know if that could have been avoided if the first doctor had read things properly but the six months I went through with him of doubting myself was horrible. I also have a huge mistrust now of ‘definitive’ scans and tests
Kelly, your timing is remarkable. I just had this happen to me! This is so scary. Too make a long story short, about five months ago I had a CAT scan of my whole body. According to my Ruemy at the time, I had RD all over except my feet. I have had difficulty walking for more than a year and some deformities in my hands. She was very annoyed with me, and told me that because I was sero-negative, I was at very low risk of deformities. My hands must be OA and nothing was wrong with my feet at all. The second Ruemy I saw seemed to be amused at me wanting her to look at the bones sticking out of my hands and feet. Then I went and got an MRI of my feet, according to the person that wrote the report said I had RD in my feet. So, when Ruemy #3 started to tell me that he concurred with #1 and #2, I interrupted, and told him I had a MRI that stated differently. His attitude changed immediately, I sent him the CD and the report.
It just seemed so dumb to tell me that I have RD all over my body, but not in my feet?
thank you for sharing this story Lynne. Hopefully it will encourage others not to give up. So hard when a doctor dismisses you without an examination or based on his/her preconceptions. So hard to keep going to another doc or challenge them to re-think it.
The first time I went to my primary doctor for RD symptoms I was 27 years old.(I’m 40 now) I said “I feel like I’m falling apart.” And her response was “It sucks getting old!” I said “Im only 27!” She chuckled and walked out of the room! That was just the beginning of a very long journey. 11 years and 3 rheumatologist later, I was finally diagnosed with RA. Funny thing though I didn’t get joint damage until I was treated with powerful meds.
You bring up many important issues here, each of which really should be addressed thoroughly at some point. Among these are the current dependence on sophisticated tests instead of clinical medicine and the lack of caring by many of todays physicians. Most important for you and all patients with arthritis of any kind that affects the weight-bearing joints of the feet, ankles, knees, hips and back is that there are always mechanical components to their arthritis. When you have a condition like RA you are “labeled”; i.e. all associated problems are assumed to be due to that disease. But in fact, many of the problems in you feet may be due to the mechanical problems we all have like pronation or a flattening of your feet. In addition, your RA has altered your mechanics (how you function). So if these issues are not dealt with, even the most optimal control of your disease cannot get you fully symptom free. The bottom line is that there is a great deal that can often be done for you and all with RA by optimizing foot alignment and positioning that is not even routinely considered. Such optimal alignment can not only help your feet but all of those weight-bearing joint they support. You would be amazed at how much better your knees for example would feel if this were done.
Lou Pack, DPM,MS,DABFAS,FACR,FACFAS,FAAAFAS
http://WWW.drloupack.com
I’ve had 4 scans and two MRI’s in the past two years and won’t have any more. Not the money, we don’t pay, but the amount if radiation scares me. I’ve made a point of collecting not only reports but a cd of the scan. That way I can get a different doctor to look not just read…ciao
This site is a God send. Nearly 20 yr ago I started having problems wearing my contact lenses and got infections that morphed into severe dry eyes. My eye doc recommended I be screened for autoimmune disorders then and at every annual eye exam. My family doc disregarded this until 10 yr ago when she reluctantly did blood test for RF. Negative. As far as she (and I) knew this ruled out everything conclusively. 5 yr ago I started getting bad hand joint pain and a trigger finger. Went for physio, therapist recommended I see a rheumy. New family doc felt this was not right move as more blood work was all negative. See a pattern here? Anyway, 1st rheumy I went to noted I had a trigger finger and basicly told me to come back when I was in more pain. Saw 2nd rheumy 6 mon later and he took me a little more seriously and said straight out that bloodwork is not 100% and just a portion of diagnostic tools available. but despite so much swelling that my knuckles were nearly invisible(no “valleys”) he didn’t see what he felt was typical RA joint swelling. Fast fwd a year and he saw something I guess and put me on plaquenil. In last two visits he says I am fine. To be sure it has helped with dry eyes/mouth and fatigue…hand pain to some degree. Bloodwork still negative. But last 6 mon I have been under severe stress at work and my hand pain and swelling is worse, my feet and ankles hurt. Can’t take naproxyn as it killed my stomach. Taking tramacet. Just flew 6+ hours for an 8 wk vacation and my hands way worse after that. New trigger finger on left hand. I see my rheumy in May…any bets on him saying I am “fine”. I am in paradise and just want to sit and read. Sorry for whining but I am at end of my rope. So very glad to know I am not only one with “untypical” results. My fam doc did send me for bone scan which she said was well lit up…not sure what rheumy will say about it. Thanks guys…feel like I am not so alone.
I am an RN who works in Oncology Pharmaceutical Research, and consistent imaging is one of the things a drug trial lives and dies by in Oncology. Lesions appear, disappear, and are read all sorts of different ways. The hallmark of a radiologist is hedging of the bets, likely malpractice based, and reports almost always contains “suggestive of”, “could be related to”, and of course the way to help themselves “further study may be helpful”. I am not only an RN, but have been diagnosed with Lupus and RA, but only after 20 years of being dismissed as someone with the problem being psychological, or merely seeking pain medication. The outstanding suggestion on this post is to keep records of laboratory and radio-logical studies. With the paper or electronic copies being shuffled about they can and will be lost.
methotrexate has been shown to ‘heal over’ some erosions, despite it not being aa cure-all. I suppose biologics have done this also in some cases.
I have had ra since I was a child. Many similar experiences. The best you can do is find a good rheumatologist and be you own advocate. Also I started Pilates with a personal trainer. She has done wonders for my feet. Strongly recommend the silly looking toe socks. They help to keep those piggies where they should be. Good luck.
I was recently diagnosed with RA but I think I have had it for at least 10 years, I have suffered tons of infections, and hip pain for most of that time, going back and forth to Dr.s. I recently had a baby, and had a awful pregnancy, my hands and wrist become impossible, and walking my last tri- was also impossible. I read that RA usually dissipates during pregnancy but not mine. Now I have very limited use of my hands and wrist and very limited with walking and other things because of my hips. I have recently filed for SS and had to go to one of their Dr.s who made me feel like I was a quack. What I tried to tell him was although I can do some of the physical test he asked me to do, I would not be-able to do them repetitively and what I do today I may not be able to do tomorrow. My question to you is, do you find this when you go to the Dr, and does your symptoms change from day to day. Some days my forearms will hurt, and some not, someday’s I’m able to hold something, and some days ‘m not. He kept asking me how long I could stand or sit, and I was unable to give him a straight answer. I told him it just depends on what I have been doing or have not been doing on that day. This is all so frustrating and I feel there is no help, its a double edge sword, If I move to much I hurt, if I don’t move enough I hurt, I don’t know what to do, or how to make anything feel better. Any advise on dealing with any of this.
I have RA but my story is actually about an injury that happened several years ago. My orthopedics sent me for an NOT of my hip. The radiology report stated that my hip was unremarkable other than some IS in the hip. Fortunately the Doctor had a lot of experience and could plainly see that one of my muscles was actually torn away from the bone. If we had listened to the radiologist it would have been very bad. I could barely walk, my knee kept collapsing as the muscles apparently all work together to help you walk. Thank goodness for a great doctor that listened to me.
THANK YOU SO MUCH FOR ALL YOUR WORK WITH RA WARRIOR. I KNOW YOU BEING A PATIENT WITH RA, THERE ARE DAYS YOU ANSWER POST WHEN YOU YOURSELF PROBABLY ARE FEELING WORSE THAN A POST FROM ME. THAT SHOWS ME HOW DEDICATED YOU ARE TO HELPING PEOPLE WITH THE DISEASE AND DOCTORS WHO TREAT US ALSO. I ALSO KNOW YOU HAVE SOME WONDERFUL CHILDREN THAT HELP YOU TO ACCOMPLISH THESE THINGS. I WAS DIAGNOSED JUNE 2011, WISH I HAD FOUND YOUR SITE BEFORE NOW. I DID AT THAT TIME BUY THE BOOK LIVING WITH RHEUMATOID ARTHRITIS, WHICH HELPED ME TO SEE I NEEDED TO FIND ME ANOTHER DOCTOR. MY SECOND DOCTOR IS GREAT.
RA WARRIOR FOLLOWER,
JOAN
After forty-four years years with this RA i’ve just about had it. No, is not an invisible disease
for me, people think i was born with these hand. I’m 76 yrs young and some days I fell a 100.
My left me in 1991 because “i live with the RA better then he does.” So he told my three adult
boys.. I had 12 joint replacement plus cancer in the pass. 23 years. Yes, i have pain every day
but manage to smile, laugh and even dance. Does my family get it no. Because i’ve always
been there for them. I have eye problems, copd(no i have never smoked). I could go on and
on but it does no good.
Third line insert former husband
I hope everything is okay! I miss your blogs!
Just got results from hip,pelvis,hands,wrists,feet and ankle x rays…normal. Labs: (-)RA and CCP. CRP up to 44 from 40 a few months ago. Started Mobic daily a few weeks ago and its helping the pain but still hurts in my feet, ankles,hips and hands. The swelling was generalized puffiness and is down since Mobic. Want to cancel my follow up with Dr as I know what she will say, “can’t possibly be RA!” This is crazy, I am losing my mobility and can’t get help. Now xrays are normal even though I have Curling of my toes. Dr quiped “yes, hammer toes.” It happend very quickly after the pain started, can this be normal??
The sad truth is that our best diagnostics still have relatively unimpressive rates of sensitivity and specificity. Inflammation makes reading some of these tests even harder. When my disease was very active, the hip specialist said the hip was severely damaged and needed to be replaced but that I should wait until the flare abated. I have a juvenile form of the disease which can experience long periods of remission, which thankfully, I am now experiencing. The next MRI said that the damage was moderate and that hip replacement should be delayed. Then I started swimming, doing yoga, stretching. I lost weight, went on one of those low inflammation diets. The next MRI said mild to moderate damage. You can see where this is going. Its not that the doctors are incompetent (although they can be). Its that we’ve been sold a bill of goods on diagnostic testing that isn’t altogether correct. They are not that sensitive (aka they miss things that are there) and they may not be all that specific (high rates of false positive). Sad to say but nothing substitutes for a reasonal doc with good common sense.
great points Kay!
just had x-rays for hip pain radiologist said it was hip OA went to orthopedic he said its RA. need a new hip! who is right who is wrong. guess I won’t know until they go in. ugh!
Two observations:
1) Plantar fasciitis like symptoms were among the first set of symptoms that I experienced that triggered my visit to a doctor to see what was wrong, and that lead to my being diagnosed with RA. My RA doctor did a full set of x-rays at that time, and now a year later a second set has been taken to see how things have progressed. I will learn the analysis in a couple weeks.
2) I hope all is OK at the Young household since there don’t appear to have been any updates to the main page in several months.
I am just trying to figure out where is Kelly? Does anyone know. She hasn’t posted for some time! Thank you.
It’s completely insane that scans, which invite error at multiple points – and each error can of course be compounded by the next – are trusted over the lived experience of the patient. I mean it’s not like it’d be impossible to at least acknowledge these things or try to amend them, but it would mean doctors would have to get over themselves.
This is what should happen (but won’t):
– Each exam could undergo review by three radiologists at different institutions, chosen by lottery. At least one of them should have more than ten years’ experience. (The validity of the reports of radiologists with experience has been shown in studies to be far better than that of residents. I mean, obviously, it would. But inter-rater reliability is low, and juniors get it wrong especially often.)
It wouldn’t be technically difficult to do this. It’s 2014. A secure file-sharing site run by their college, maybe, a randomization procedure, an email. “Here Dr. X, is a link to your five “second look” scans for today.”
I was a proofreader once. We had three pairs of eyes on a bloody news release before it went out.
I just discovered your blog while doing a search for rhuematoid arthritis. You see, my husband of eight years just got diagnosed with RA. He is 32 (I’m 30) and we are still in shock mode. But we are glad to finally know where all his health issues are coming from. Dr gave us a list of DMARDS to choose from and we are leaning towards sulfasalazine… we know that its going to be trial and error for a while with the meds. I guess my question for you, and anyone who reads through the comments, would be – what can I do to help my husband? Do you have any tips as to what I should or shouldn’t do? I have been by his side through this and we talk about his pain levels (1-10) everyday. I want to support him in every way that I can!
Gosh, I can relate!!
I haven’t seen an update to the RA Warrior blog since this one on Feb 4. Is it still active? I may have fallen off the “subscribe” list.
I hope Kelly is okay!
Hi Kelly, Thinking of you and missing your posts these past months. Imagining that you may be catching your breath, being with processes related to your RA, and tending to self-care.
I just wanted to send you the best of wishes and prayers and thanks for all you’ve done and been doing in the chronic illness community (I have CFS but still love your blog).
The pics of your feet could be mine except that my curled toes are on the left! My Dr said something about “hammer toes” and then went on to tell me about arch support etc! I also had negative x rays, but the report said no earlier studies to compare…I had bilat hand and wrists x rays a few years ago in the same department. Also seronegative and Dr never agreed with the swelling. This week my feet and ankles hurt so badly I wanted to crawl and this time my ankle swelling was remarkable. I took pics with my phone and made and appt. Suddenly the light went on with this Dr! Swelling and warmth to both ankles,wrists and fingers! Although, my fingers looked the same as they did 2 weeks ago when she saw no swelling! The boxes are ticked, I finally started on prednisone with further treatment expected with methotrexate or Plaquenil dependeding on the latest lab results. She now says either RA or inflammatory arthritis, which I cant seem to find what the difference actually is.
Hi my name is marcus, i’m from london UK, i had the same thing with my rheumatologist, as i have had RD now for just over 2 years, about 4 weeks ago i had a bad flare-up on my right foot, i went to my GP and he sent me for X-ray, and when i seen my rheumatologist a week later i asked him about the X-ray his words!! i have degenerative disorder of 2 of my toes, and he said the same as the OP said we all get that as we get old, (get old i’m only 43 also!) think its time to find myself a new rheumatologist!
It is a challenge. But, I would say scans and xrays do not necessarily correlate to pain…and was told that by my specialist. And, he was right. Because my pain is less than it was…even though there is no improvement obviously in scans.
I have also found that digital imaging is a computer interpretation of what the matchine sees. Digital images tend to shadow sometimes differently and then sometimes it is just a doctor doesn’t know how to read them.
I am in turmoil after a visit (my third) to my rheumatologist today. She said my lab results are normal and she sees no inflamation on examination and therefore, she beleives my RA is dormant. I am still in pain (hands, wrists, ankles, hips shoulders) and have experienced only minor relief from a new biologic drug. She even hinted that my diagnosis may be incorrect – I was diagnosed with RA by another Dr who has since left this medical practice. I told her after a particularly demanding week at work last week every joint in my body was on fire by the end of each work day. She said she had no idea why that would occur. She observed that I suffer from anxiety and depression and asked if I suffered from fybromyalgia (sp?). The implication I drew from her comment was that this is all in my head. My pain is in my body, my joints, not in my head. I feel dismissed and I’m even beginning to doubt myself. I can’t stand for any extended period of time, and I can only walk short distances before joint pain forces me to sit. I am so upset I don’t believe I can go back to see this Dr. again. I’m wondering if anyone else has had a similar experience with a Rheumatologist.
Yes Marie, I think many have. And I’ve had it too many times as well.
Can anyone tell me if severe pain and lameness in one leg could be RD? I have been diagnosed with severe? RD a year ago but up until a few weeks ago I could walk. I am on methotrexate and prednisone. I try to stop the prednisone but cannot because the pain comes back with a vengeance. Now when I put weight on my right leg the pain is pretty bad. My doctor just said it was my hip and let it go at that. I am guessing he cannot or will not do anything to help? I can just get around with a cane. Does anyone who might be reading this have any ideas? or similar symtoms?
Ann, I’m sorry about your leg. It’s hard to know from here what the cause is. It could be rheum inflammation in your hip & it could get better as a flare subsides or it might improve with an injection of steroids in your hip. But sometimes a lame leg is really a spinal symptom. So you may need to see another doctor so you can get a better answer. Do you have an orthopedist you can see or maybe you can call your general physician and ask her/him who they recommend.
Yes, I’ve had lameness last for a few days at a time from the hip flares & the rheum dr called it bursitis from my RD. But you need to be sure.
Thank you for your reply. I am just having to deal with this whole RD issue and as it progresses I can’t tell what is the disease or what might be a reaction to medication but my leg issue could be my spine as it is being affected now too! I will ask my GP what he thinks. And thank you for all the information on your website. It came up first or second in my search for this issue. Kudos to you. I will be spending much more time reading what you and others have to say about this terrible disease.
I’m 53 yrs with recent DX of RA 9/2014 but per my observation my initial symptoms began 2005 and has been an insidious course until the past 18 months which then became accelerated. I was searching for an answer to my question, how long does one have RA before erosions show on plain film X-ray? I finally found this article. I don’t know if anyone else has read it but I’m sharing it since I think it has info that might help others with an insidious course, possibly negative labs and normal xrays.
The new Rheum I saw last week, since I’m relocating soon, informed me that with the chronicity of my symptoms I couldn’t possibly have had RA longer than a year or so since I do not have any bone erosions thus far on my xrays. The article discusses 3 subgroups with RA group 1 has bone erosions that continue despite treatment, group 2 develops erosions but remain stable over time, and then group 3 those that do not present with early erosions even after a period of 2 yrs.and longer in some cases. There’s considerably more information in this study but it did support what I feel has been going on with my situation. Hope it give others some answers as well.
http://rheumatology.oxfordjournals.org/content/early/2011/03/28/rheumatology.ker129.full
That’s very interesting Susan thanks. Also, the xrays we use now are much weaker than decades ago and erosions tend to not show up on them I’m told until they are severe. So erosions may be beginning and we might not see it for a while on plain xray.
Yes, Kelly I thought it so. It would help explain why so many seronegative folks(some positive too)and/or folks with no bone erosions on xrays but have symptoms months to years before being diagnosed. I hope that makes sense! What I’m saying is that some folks suffer with symptoms a long time before getting a diagnosis and still have no erosions but it’s the other cumulative symptoms that often help establish the diagnosis, hopefully.
The new rheum I saw was adamant that I couldn’t possibly have had RA for as long as I think I’ve had it. She thinks that all my symptoms prior to a year or so are due to osteoarthritis. I understand you can have both but only 1 x-ray, my L/S spine, actually states in the report that it’s osteoarthritis. My feet and hand x-rays read as normal so how can my symptoms be osteo, since 2005?, even osteo would be present on x-ray by now! I could barely walk up to a month ago until I started methotrexate which I’ve had a good response to and no noticeable side effects. Thank goodness! I will be searching further for another rheum in my new city.
Thanks for this site and all the hard work you’ve put into it! It’s been invaluable!
Susan
I marked the study look at more later. I think it said about half of those they thought to be non erosive agree 2 yrs were seropositive. (I’m using phone right now but I think that’s what I read this a.m.).
I had the same thing happen. I was in so much pain and knew something was wrong. The first doctor said you don’t have RA but I need to do carpal tunnel surgery. He was rude and snobby. I am smart enough to know that carpal tunnel doesn’t feel like the pain I was having. Finally went to a different specialist. The first blood work didn’t show positive but a few days later I called him said I was having trouble even lifting my arm. So he did more blood work and a complete bone scan. Needless to say I lit up like the 4th of July. Oral meds did not help so I am on Enbrel injections. I stay sick with something all of the time and am still in pain. I have increased my injections but some days are unbearable.
Lisa,
I’m glad you found another doctor who would pay more attention. I’m sorry it’s not working well at least yet.
I wonder why we read so many people have similar experiences (“still in pain” & “some days unbearable”) when we are told everyone does well on meds.
The only 2 things that almost cure RD in some circumstances, as in the Netherlands, are early diagnosis and treating to target. Neither are done in the U.S. very often. And it seems that the reason is that doctors are taught to be dismissive. Anyone reading this site knows I think that is a travesty.
I was in a car accident. I told them my arm and hand didn’t feel right. It was hurting. I went a month with a broken arm. The radiologist read wrong. IT was CLEAR when i even saw it that it was broken. Now i’ve had an MRI because the places where it’s not broken, hurt worse than where it is broken. the Mri says unremarkable and negative….I don’t agree. Although, my ankle that i’ve had discomfort with, shows some bursitis. Since my original xray of my arm was done wrong, not once, but twice…the night of the wreck, and the next week at the dr office, both sets of xrays were read wrong and i was told i only had bruising….how should i go about asking if this is right? Should the Orthopedic doctors be able to look at it and tell anything?