Chest Pain in Rheumatoid Arthritis: Costochondritis Anyone?
Severe chest pain can send you to the ER – unless you know it’s “just” the Rheumatoid
 This past week, someone turned up the volume on my chest pain. I was glad I’d heard other patients say they went to the ER for chest pain and it turned out to be “just” costochondritis. Maybe that prepared me so I wasn’t frightened when it happened to me. The chest pain has gotten severe, and it joins the chorus of the shoulders, knees, neck, hands, wrists, and toes… A chorus of disharmony.
This past week, someone turned up the volume on my chest pain. I was glad I’d heard other patients say they went to the ER for chest pain and it turned out to be “just” costochondritis. Maybe that prepared me so I wasn’t frightened when it happened to me. The chest pain has gotten severe, and it joins the chorus of the shoulders, knees, neck, hands, wrists, and toes… A chorus of disharmony.
Costochondritis is not new to me. The first time we met Dr. Smart, doc pressed on my rib joints and asked, “Is that tender?” Surprised to be asked that, I said, “Yes.” Doc said it’s common with RA. Really?
Common like cricoarytenoid joint arthritis (which doc didn’t believe in)? Or like ear pain? Or neck inflammation? Or shortness of breath? Or other Rheumatoid Disease-caused problems we don’t know what to do about?
(Doc never doubted my DIP joints though – and injected one of them with steroids.)
Costochondritis: one of the neglected Rheumatoid symptoms
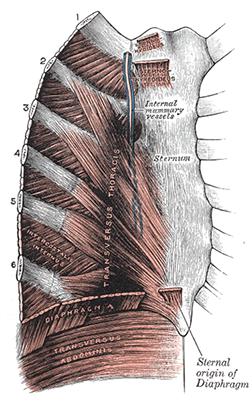 As early as 1964, the journal Radiology published a study explaining that the effects of Rheumatoid Arthritis on the rib joints “have not been adequately described in the literature.”[1] Mayo Clinic’s description of costochondritis makes it clear the word describes a symptom, pain or inflammation of the rib joints that can be caused by various illnesses.[2,3] The term is also confusing because there can be varying diagnoses with similar symptoms, as you can see in the Medscape costochondritis diagnosis page.[4]
As early as 1964, the journal Radiology published a study explaining that the effects of Rheumatoid Arthritis on the rib joints “have not been adequately described in the literature.”[1] Mayo Clinic’s description of costochondritis makes it clear the word describes a symptom, pain or inflammation of the rib joints that can be caused by various illnesses.[2,3] The term is also confusing because there can be varying diagnoses with similar symptoms, as you can see in the Medscape costochondritis diagnosis page.[4]
But I’ve also read some skeptical articles about the symptom, to put it politely. Costochondritis is considered by many a garbage can diagnosis or related to hypochondriasis.
Costochondritis is sometimes distinguished from Tietze syndrome because the latter has swelling. However, as we’ve learned, inflammation often includes inconspicuous swelling. I suspected my own rib joints were swollen yesterday, and compared to how they are now, I’m certain of it.
With the many common RD mix-ups like this, my solution is to specifically describe what’s happening, especially when talking to a doctor, and leave out the hot-potato word. Without thinking, that’s what I did in my inventory post: it discusses ribs along with clavicle inflammation, but doesn’t say costochondritis.
Costochondritis obviously does exist.
Like many things in medicine, it is doubted or mocked by some because too little is known. And it is all too real to people living with inflammatory diseases that attack joints.
Costochondritis is treated, like other joint inflammation, by rest, NSAIDs, ice or heat, and prednisone. Pain medications can help manage severe costochondritis. And if it is persistent, steroid injections can be used. Usually, as with other joints, the inflammation subsides to a more manageable level in a few days. I’m counting on that because the only other solution I can think of is to not breathe. It hurts too much.
Have you had pain where your sternum meets your ribcage? Did you ever notice swelling? What did your doctors say?
Recommended reading
- Inventory of Rheumatoid Disease: One Patient’s Experience
- Sternoclavicular Joint Involvement in Rheumatoid Arthritis: Fascinating Discovery of a “Neglected Joint”
- Should Chronic Pain Patients Be Treated in the ER?
- Traveling with Chronic Illness/RA Part 2: 20 Helpful Tips
FOOTNOTES
1 Alpert M, Feldman F. The rib lesions of rheumatoid arthritis. Radiology. 1964 May [cited 2013 Aug 27]; 82: 872-875
2 Mayo Clinic [Internet]. Costochondritis. 2012 May 6 [cited 2013 Aug 27]. Available from: http://www.mayoclinic.com/health/costochondritis/DS00626
3 HealthHype.com [Internet]. Severe costochondritis – causes, symptoms, treatment. 2010 May 9 [cited 2013 UF 27]. Available from: http://www.healthhype.com/severe-costochondritis-causes-symptoms-treatment.html#more-8619
4 Flowers LK. Medscape [Internet]. Costochondritis. 2012 Apr 13 [cited 2013 Aug 27]. Available from: http://emedicine.medscape.com/article/808554-overview
5 Wikipedia contributors. Costochondritis [Internet]. Wikipedia, The Free Encyclopedia; 2013 Aug 23 [cited 2013 Aug 27]. Available from: http://en.wikipedia.org/w/index.php?title=Costochondritis&oldid=569906531




I have finally found an RA doctor. But he seems to think none of the symtoms are related to this disease. I suffer from Neropathy in my feet. And of late muscle spasms through out my body. My legs , feet , facial, neck and stomach at times. Does anyone else suffer from this? It is horrible and wakes me up. I walk the floor..put heat on it and it goes away. This is new to my RA. And the search to even find out what was very frusterating search what was wrong with me was a very long search. When I have a flare up I take the predisone. And I finally take methotrexate very low dose. Have been taking it since May.But for pain….which is not bad any more… except the muscle spasms. Please share if you have these symptoms.
Hello Susanne. Yes, I suffer from those symptoms as well. My Rheumy isn’t sure what it is or why I have it, but she added gabapentin (sp) to my cocktail. It has helped. Though, it’s really a weird sensation to feel those things isn’t it? Good luck!
I hope your new doctor works out Susanne! Yes, neuropathy is common with RA. Inflammation inside of joints that can put pressure on nerve pathways or affect circulation; also joints in the spine can be affected, causing neuropathies in hands or feet. Hopefully you mtx and prednisone will help it.
And muscle spasms or tendon cramping – yes. Talk to your doctor; a low dose of a muscle relaxer might help when it’s really bad.
I’m so glad I found your blog. Recently I went to the ED because I thought I had a pulmonary embolism. After a dozen of tests, I was diagnosed with Costochondritis. It took several weeks for the chest pain to subside. I was initially diagnosed with RA over 10 years ago and was in remission until last year.
I have had this type of pain . Methotrexate didn’t help, but adding hydroxychloroquine worked wonders!
Today I had such sharp pains in my chest … could not take a deep breath. I have told this is a conditon of inflamation and it will not kill me. But when it happens it feels like a knife in my heart.
Does anyone else suffer from this?
yes, like Mandy said, it can be very sharp & now I see why some have gone to the ER thinking it was a heart attack. Of course, if you have any other symptoms that make you concerned it’s really a heart attack, get it checked out.
Two years ago, overnight, a painful lump developped on my chest, close to my left breast. It was indeed painful, so after two days of “coping” with the pain, i went to see an uninformed doctor, who Even when told I live with RD, thought I had a breast disease and sent me urgently to a breast surgeon… The breast surgeon, luckily, had a daugther with JRA, so after very careful listening to me, and extra careful and gentle examination told me it was “just” costochondritis.
My second encounter happened a year later, when sudden pain on the right middle side of my rib cage left me breathless. This time, i went straight for the ER! The intern asked: had you ever had costochondritis? Right from the start!!! So a few pain meds later, I was released. It is a fast and furious condition – hopefully it will not last for very long, Kelly!
When I first had this chest pain I went to the emergency doctor at the health centre. I told her I had a really bad pain in my chest and it was very tender to touch. She decided it was nothing as she couldn’t feel a breast lump! So, I went to the ER at the local hospital. I was given pain relief and sent for an xray whereby I was diagnosed with Costochondritis. The doctor was very nice and explained it was related to the RA (as if I didn’t know!). The article is excellent for anyone who hasn’t experienced this pain yet.
Good morning warriors. This is my first post. I have been reading RAW since being diagnosed in October of 2012. I just wanted to say that costochondritis was the very first symptom of RD I ever experienced. This was November of 2009. The pain was horrible and I thought I was having a heart attack. I was told at the ER it was “only” stress. My pain never went away and only became worse. A year later, Sept 2010, I was diagnosed with FMS. It wasn’t until I found a wonderful Rheumy in 2012 who finally diagnosed me with RD. I still have the chest pain from time to time. My collarbone has now joined the party. It is probably the pain I dread the most. I understand how scary it can be.
Kelly I just got done having lots of tests because of the pain. Thought it was my liver! So did the doctor. All came back negative ! Then I see this post! A lot of the time it only hurt when I bent over. I just can’t believe a gastro doc couldn’t figure this out. Now I have a answer! Thanks again for your help!
yes, it can be a lot worse when moving. glad your liver is ok Judi.
I had this start in january. I freaked out thinking it was a heart attack and went to the e.r. They ran all the test EKG , blood gas (ouch!), chest x-ray, ect. After several hours and a breathing treatment they said it was asthma….the next night it was back again really bad. The pain comes on so quickly you think your having a heart attack so I went back to the e.r. They did a chest cat scan, then told me they believed I was having panick attacks, gave me Xanax and sent me home. I thought I was going nuts because it wasn’t just the sensation of not being able to breath but there was pain and tenderness. So I researched and found costochondritis. I went to my rheumy (who is wonderful) got halfway through my ordeal at the e.r and she knew what it was. It’s horrible. Every time I have it I worrie about if it’s a heart attack or just my R.A……I am only 34. I am glad to hear I am not crazy and others experience this too. ( the E.R. Docs acted like I was insane). But sad at the same time that others are also suffering. Stay strong!
I have had many rounds of having sharp pains when I breathe and pain throughout my ribs. But mine is never near the sternum, it is across the back of my ribs. I was told I had Pleurisy, this keeps happening over and over and over…each time I am given a steroid pack and instructed to double my NSAID for 10 days. I wish I knew how to kick it, it just keeps coming back. I also had an ER trip last week for severe pain deep in the left side of my neck and the ER doc pressed on the joints where my clavicle meets my sternum and it was excruciating, he said the Rheum inflammation there must be pushing against the nerves in my neck. Steroid pack again. Has anyone else had these things? Thank you as always for your wonderful page!
I have had occasional rib pain that comes on out of nowhere to just stop me from whatever I am doing. The pain is sharp and I must be careful when I move. I also have neck pain which proceeds across my shoulder and down my arm. The rib pain is a recent occurence.
I like my Doctor but he seems deaf to neck pain.
Thanks for having a place to vent.
maybe you can find a pain dr. or an orthopedic who knows about rheumatoid – to help you with the pain treatment.
Hi, all, I get costochondritis periodically and it is definitely scary. I’ve gone to the ER a few times; after the first time, I tell them what I think it is, but that since it’s difficult to differentiate from the descriptions I hear of heart attacks, I need to rule that out. They seem to accept that I’ve been through it before and know what I’m talking about, and ruling out a heart attack is a reasonable request (mind you, this is in Canada).. I get checked out enough to put my mind at ease and rule it out, without being put through a battery of unnecessary tests. I grab a book to bring because the blood test results can take a few hours. Of course I only go when it’s really bad and I can’t say for sure that it’s “only” inflammation. I find a warm bath helps, as does my heating pad. I stop trying to work because computer posture makes it way worse and I know my body is telling me to rest. This is a very scary symptom! Don’t be embarrassed or minimize your pain… Better safe than sorry!
The first time I had costrochondritis it scared me so bad. It was long before I was diagnosed with RA. But ever since I have had RA, I get it quite frequently. Still is scary sometimes because I have high bp. And yes, it sure can hurt. I’ve been diagnosed with RA for about 3 years now and I still get busy doing things and forget how tired I will be in just minutes sometimes.
This post and the comments about costochondritis is another example of how misunderstood RA is.
I am wondering if there are avenues for how patients can inform a group of doctors in our local areas about all the ways that RA can manifest. I know that some doctors get insulted when patients presume to know medical information that doctors feel should only be shared among doctors. I’d love to see a patient-driven collection of talks or printed materials or this information prepared in a format for educating doctors and other medical professionals on a website ! Topics I can think of from the patient experience are:
1. Diagnoses (the difficulties we’ve had or heard about and then what we’ve learned about the diagnostic protocol)
2. How RA can and does manifest in patients (all of the symptoms that the research shows is related to RA, all of the associated conditions)
3. Tests for RA: bloodwork and imaging
4. Treatment: it’s not ok to just send us home with pills and ask us to come back in 3 months. Comprehensive treatment- physio, OT, therapeutic pool exercises, social worker, vocational rehabilitation, counseling, referral to other doctors, cortisone shot, support groups
5. Monitoring Disease Activity: pushing on joints isn’t enough, bloodwork isn’t always accurate to monitor disease activity, x-rays are becoming obsolete, patient reporting scales should be standard practice, use of advanced imaging
6. Needs in rheumatology from the patient perspective: increased research funding for a cure and to better understand the pathophysiology of RA, funding to improve the number of doctors training as rheumatologists, approval of advanced imaging by insurance companies, improvement in information taught in medical school for rheumatologists about what this disease actually is and how it manifests
..yes, much of that is covered in my new toolbox for healthcare professionals – I think the online version is a first step.
(By the way, coming back in 3 months would be an *improvement* to the care many receive. I’m pressing for them to even be aware of a 3 month guideline.)
We’ve discussed this stuff at length in the past & I’ve got to get offline & do a full day’s work – but I wanted to take time to say that many more people know & care about this now than ever before. There is hope! Some do get good care & we will hold their example up & as long as patients have a choice who they see, they will navigate *away* from the uneducated or dismissive “care.” My upcoming book is aimed at educating the medical profession particularly so more to come on that! You are right to realize how important it is to patients – we may become educated, but we need educated clinicians to work with us.
One of my first symptoms was costochondritis. The doctor told me that some people just get that for no reason. This was the same doctor that told me that all of her patients complain about fatigue. Needless to say, I don’t see her any more! This is still one of my most common symptoms. When my son sees me rubbing my chest he says, “Do you have that Costco thing again?” The good thiing about it is that I know my heart is healthy! It gets checked pretty often by doctors who want to make certain it’s not a heart attack.
I went to my family doctor with excruciating pain in my left ribs, he diagnosed costochondritis. He told me all that could really be done for it is heat and something for the pain.
I have added a long-line posture bra to that mix. It gives just enough compression that I can move if I have to (albeit very slowly)
I’ve had chest wall, rib & sternum inflammation since day one of my diagnosis sixteen years ago. My rheumatologist always acknowledges it at each visit and examines the area which is always noticeably (at least to her trained hands) inflamed and, of course painful and tender. In January of this year, I had a “different” kind of chest pain that was more stabbing/shooting pain that traveled up toward my neck. Smartly, I did not ignore this and, after five days in the hospital, was diagnosed with a heart defect likely related to the RA and years of inflammation. You must know your body well and do not ignore a change in chest area pain.
I was diagnosed with RA 9 years ago and sadly to say, nothing I have tried has put me into remission. Therefore I have had to really get to know my body and sort out day to day ” what is RA related and what is not”. I had my first bout of costal chondrites about 3 years ago. My Rheumy dx it and treated it with Indocin but it really never resolved completely. As most of us, I just learn to “roll with the pain” when it’s not horrible. I am an RN for 35 years and have seen it all but one day on the unit I was on the phone taking an order from a Doctor and suddenly experienced THEE MOST EXCRUCIATING PAIN RIGHT IN THE MIDDLE OF MY CHEST! Luckily the Nurse Manager was standing right next to me and I told her ” Nicole I’m having chest pain”! I could barely breathe and it was increasing by the seconds! She took my BP which was 220/102 and my pulse was 140, I was sweaty and clammy and pale. She immediately called a ” Code for employee in distress” and I was whisked down to the ER within seconds. I am 60 years old and female and with cardiac disease being very high for women fortunately the Physicians in our ER took this very seriously. I will mention that this hospital is a major Trauma Hospital and the #1hospital in this state. I was worked up for cardiac complications and kept there overnight in the cardiac observation unit and thankfully nothing cardiac was involved….BUT I was still in pain dispite the morphine I was given for pain. I was sent home with them saying ” we may never know what it was” . I went into see my Rheumy who did not have privileges at this hospital and he truly was remorseful that I had suffered and was still suffering with such pain. After examining me he diagnosed Tietze’s and over the course of three days I was injected with 24 INJECTIONS into my sternum and ribs from my clavicle to ziphoid process with prednisone and lidocaine. Believe me…compared to the pain I was in the injections were NOTHING! This took the pain away immediately after the third day and sadly after being totally free of the pain…I realized just how long I had been suffering with it. As most of us RAer’s we get used to not complaining about ever little pain BECAUSE WE ARE ALWAYS IN PAIN and truthfully….I just get tried of complaining…or trying to prove myself. The sad thing I have realized is that doctors other than Rheumys HAVE NO CLUE about RA or its symptoms!!! Costralcondritis is VERY REAL AND VERY PAINFUL and it takes awhile to go away! I still recommend that if you are experiencing chest pain of any kind to GO TO THE ER……but if you are cardiac cleared and still not having relief, talk to your Rheumy about the possibility of costralchondritis or Tietze’s ! Sadly after all the pain,suffering and my own very and anxiety that I was experiencing a heart attack, when released from the hospital and family and friends asked ” what was it?” I had to say ” they don’t know they couldn’t find anything”. Once again I had to endure the rolling of the eyes and side ways glasses of those that still think “I’m bonafide crazy”!!!!!! God bless all of us that suffer with this HORRIBLE disease that is so underestimated, so unbelieved and so ignored by much of the medical professionals!
Kate, what an incredible story. Thank you for your post. I am becoming passionate about how each of us can make a difference to improve the awareness of all the manifestations of RA so perhaps the next generation won’t have to face the stigma, the eyeball rolling, being made to feel crazy, and in the most extreme cases – dying from complications of the disease. It’s one thing for us to share our knowledge among those who suffer from RA, it is another to impact the medical professionals and the general public. I’m just finding my way on how I might personally make a difference.
I firmly believe RA Warrior and Kelly Young’s impact on the general public’s and medical professional’s awareness of RA is nothing short of miraculous. I can’t imagine where I’d be personally without RA Warrior.
Funny. ..I brought up this exact pain to my rheumy last week and her exact words were “ribs are not affected by Ra”. REALLY!
I have had frequent pain and inflammation right below my left breast on the rib cage for around a year now. Sometimes it gets inflamed enough to see it, like if I had a hot kind of squishy golf ball in there. Thank goodness it doesn’t hurt to breathe and I’ve never mistook it for a cardiac event. It does get worse if I do something physical while sitting at my desk, like collating or using a paper cutter. I know it’s my RA because it gets worse when everything else does. Just thought I’d share my experience, which thank goodness is more annoying, unlike some of my other symptoms that can make me completely miserable.
Hi,
Does anyone feel weakness or off balance with RA? I have it everyday, Dr say its stress. I’ve had an MRI it was clear. Thx
I spent an unpleasant night in the hospital in June from costochondritis. I had never heard of it till then. My GP did a much better job of explaining it to me than my rheumatologist. Too much activity now causes crushing pain.
Luckily, I found a Rheummy who believes in costochondritis. He even identified it for me because I was frightened of the chest pain and the pain under my breasts every time I stretched or twisted a little bit. It exists, for real — I know; I have it!!
I recently had several days of chest pain along both sides of the upper sternum. Not a usual place for me to have pain, but it was tender to the touch, which made it pretty certainly inflammatory. More commonly, I have had pain at the lower end of my rib cage, around the clavicle/collarbone, and frequently during a flare have scapular/shoulder blade pain which can be severe and sharp and worse when taking a deep breath. Never noticed swelling, by the way, though never really looked for it in these areas.
This reminds me that my primary physician recently said to me that I am doing quite well except for the RA/RD and its complications. Ha!! Yeah, only the symptoms and side effects that affect almost every joint, muscle, tendon, and bone in my body as well as multiple organs and systems!
YES! I’ve been waiting for a posting on costochondritis. I’ve suffered with this for at least twenty years and need to point out that it is also weather-related. In extreme cold (winters in the NE) I’m inflamed and my chest hurts so badly I can hardly take a breath. I’ve tried NSAID’s, heat, ice, rest. I can tolerate intense pain, but the maddening part of this is that no one seems to acknowledge the connection with RA. They just don’t know. Having had a hx of upper mantle radiation for Hodgkin’s Disease many years ago, my hem-onc thinks it may “just” be scar tissue. And that may indeed be a contributing factor. I, however, am certain that it is related to my R.A.. The profoundly sad thing is that in addition to tolerating incredible pain, and whittling away the activities in my life, I’ve had to wonder about my sanity because NO ONE acknowledges the chest pain unless they have something to offer. I don’t need to feel crazy and a simple acknowledgement would help. So thanks for posting.
Laurie, I wish more doctors read this website. I see a rheumatologist at a hospital ranked as one of the best for rheumatology (if you are to believe US News and World Report), so in theory she should be one of the best docs out there, but I have stopped mentioning any non-joint symptoms I have, because I think I will lose my mind if she tells me one more time that RA doesn’t do or affect this or that. I can tell I lose credibility with her every time I say something, and I can’t afford to move on to another doctor, so I would rather stay quiet. It totally sucks.
Gwyn, my hope and prayer is that our generation of RA’ers will find a way to make a significant impact on the ignorance that exists in the medical community as well as with the public. I’m SOOOoooOOOO sad to hear that you feel and know that you have to remain silent. I’ve experienced the same thing.
I know RA Warrior is doing a wonderful job (that’s a bit of an understatement !! ) in providing information just as fast as they can. Kelly just mentioned that she is developing an RA toolkit and I know she’s in process of writing a book.
I don’t know what strategies we personally can employ to help correct misinformation and educate the medical community and public in our own communities. I’m trying to brainstorm ways I might have an impact locally on exactly the situation that you describe that happens thousands of times a day in doctors’ offices all around the world.
We have SO MUCH knowledge now about RA – there is so much published research on all the manifestations of the disease and RA Warrior has been instrumental in changing misperceptions. I was a researcher before RA literally destroyed my career in a very short time. As I am able, I’m using my research skills to understand the disease and collect research studies about all things RA. I’m not yet clear on how I might offer this knowledge to my local community.
I want to continue to raise this topic as a tide seems to be turning and I truly believe we all have a responsibility to help advocate for what we know is accurate information. It might just save a life or cause less suffering for ourselves and for others.
I’ve had this off and on for years, including right now. Mine is high enough that “heart attack” didn’t even cross my mind. It’s in the category of things I wouldn’t mention to a healthcare provider unless directly asked, for fear they would either overreact or check off another box in the “nutjob” column.
I have had this forever. When I get massage we pay close attention to that area. But I am always tender between by rib attachments to the sternum.
Mine never really goes away. It waxes and wains. It makes it difficult to sleep. There are days when breathing is hard. I’ve had this for years. I gave up talking about it because the Dr’s really didn’t believe me. Long before RA diagnosis. It wasn’t until my current Rheumy told me what it was. Her take on it is seen more when you have Fibromyalgia and the Fibro is uncontrolled. That is me. I’m out of control. :/
Yup, agree completely. Fibro on top of everything else is a terrible place to be!
When I stretched (which is supposed to be good for you), the costochondritis would bring me to my knees in pain! If you will pardon, it was even hard to twist to take care of personal needs. The pain would bring tears to my eyes!! It’s amazing – although I have AS, I have many of the same symptoms as RA and am on the same meds as RA. This is why I don’t miss a post on this blog!!
I had costochondritis in January 2007 and was diagnosed with RA in November 2007. I believe it was my first RA related pain. I felt like I had a box of encyclopedias on my chest and that someone was giving me a bear hug at the same time. I spent 2 nights in the hospital doing the whole cardiac workup..including stress tests. They finally diagnosed me with costochondritis. Problem was, I picked up a bad stomach flu (I spent the first night in a triage area and the lady two beds down was vomiting all night..guess what I was doing the first night I came home???) I can tell you that vomiting with costochondritis was seriously one of the worst pains ever! I have had this off and on since then, but at least now I know what it is. The only thing that helps me is meds and my heating pad. This and the jaw are my two worst areas for my RA to flare up in my opinion!
Thank you so much for the responses! I was 12 the first time I had chest pain. My care taker at that time took me to the doctor and he pushed between my shoulder blades and I cried. Every time I would swim… this pain in my chest would happen. He said I had bersitus.
But the pain was like a knife in my heart. Through out my life
it would come and if I waited ,breathed shallow it would go away. Then the ankles hurt and the wrists. The fatigue. I was known as a hypocondriac. Once went to a doctor because I was hurting all over…. and he said that was impossible. And dismissed me from his practice. Because he thought I wanted pain medication. So I went to the ER and thankfully there was a Dr. on duty who over heard me. He told me about this type of chest pain and explained what he thought I had. RA. I had thought that was just .. arthritis.
But where I live in Alaska getting into and RA DR is hard. So I flew to Seattle. He did tests for two days put me on predisone and it helped. But wanted to put me on chemo.
I rejected it and went back to Alaska. My personal physician had thought I had RA but wanted a specialist to diagnose it. 8 years ago my feet just went numb and the pain was horrible. I suffered from that until last year when my DR put me on gabbapenten. I found an RA doctor up here finally. But every thing I tell him he says that is not from RA?? Yet I have had to have a shoulder replaced.And scheduled for knee replacement. I have woke up unable to get out of bed. With some long long conversations with my DR… she is a patient woman. I finally started to take methotrexate ,a very low dose. I have only had two flare ups and go on predisone when it happens. I am seeing pain management DR. who thankfully has been around a long time and explained my RA to me. I am learning to recognize the sypmtoms. But recently since I have been on the methotrexate (since May) I have woke up at night with horrible muscle spasms. It is awful. But my RA DR says nope that is not related. A heating pad really helps. And a muscle relaxer. After posting here so many have validated this for me. Thank you!! I just get so frusterated with The RA guy. But he has helped me with the methorexate and predisone. Today I researched more and found out that I need to add magnisium and calcium to my supplments. I am now 64 and it has been a long road. I have a very understanding husband who is interested in my health and has researched with me as well. I know this was long…and I hope it helps someone. This site really helped me.
Suzanne, you have certainly been through a lot and having a Dr think that you are drug seeking is one of the hardest “external” (non RA)events possible. I am fortunate to have a dr who really understands RA, but I know that when someone does not believe your pain you begin to wonder how to behave in order to get relief. It creates a very difficult environment and causes a lot of emotional stress, which only makes the pain worse. I hope the pain management physician is able to help you.
I wanted to tell you that while Methtrexate is used in cancer treatment it is probably used more for RA than Cancer. I practiced Oncology nursing for 12 years and can tell you that Methotrexate is not used in treatment of very many cancers but widely used in management of RA. Some physicians will describe MTX (methotrexate) as a chemotherapeutic drug however Chemotherapy means “chemical” (drug) treatment. Actually Prednisone is used much more often as part of a Chemo regimen than MTX!! I know many people do not want to take MTX, for their own reasons, personally I do take it in a pretty high dose and I am very happy because it helps me a lot. Good luck as you sound like you have finally found someone to help you. God Bless Jan
I just went to the Dr. with pain in my chest a couple of weeks ago. I felt terrible, my blood pressure was so low (decreased activity, no doubt)and I had pain in my shoulders. It hurt to take a deep breath.
The did an EKG and I was having prolonged QT which sent me to cardiology again. I have had a couple of test done and I think they are ok.
My Primary Dr. put me on prednisone just incase it was RA. I am glad he did, I felt better in a couple of days.
So, yes…I have had this. It hurts.
Thank You for your help, I really do appreciate it.
Just wanted to chime in to say years before I was finally diagnosed I was diagnosed with this. I too thought I was having a heart attack. It’s very painful.
I’m kind of like Lee in that I’ve had continuous rib pain for a couple of years. The pain is at different levels everyday. Waking up is so much fun as I immediately get to find out what parts of my body are holding a party on that particular day!
I’m lucky in that the pain has not impeded my breathing in any way. But, the pain can be pretty severe in my ribs at times.
Good health everyone.
I to had this manifesting its self as pain in between shoulder blades and sometimes in front of chest too. Just like a knife is exactly how I had described it. It had it been quite severe off and on for a few months before I upped my mtx, just like all the other joints affected, if I could get in the perfect position and never move, it was fine (who likes to be imobile tho?? 🙁
Incidentally, I had had it once and awhile prior to diagnosis, always thought I had strained a muscle, little did I know it was a joint. I was always concerned that it was a lung issue too. Sometimes it’s so hard to describe whats going on there, I can be so much more specific with my wrist for example. This morning I am having my first official wrist flare after being symptom free for 7 months after starting enbrel. Thought I would celebrate by logging on and reading a little. Thank you Kelly for being my go-to site for information. Just wish it was my dr no offense:)
Have been experiencing rib pain in ribs right and left that go around to back. Have had full cardiac workup and stress test which were negative. This has been going on since my husband passed away in January. Some days are better than others with pain. Today is excruciating especially right side which I think is attributed to what I did yesterday. Finally have gotten in to see a Rheumy since my blood tests have came back positive for RA twice. He sent me for X-rays and blood work which I will get the results on Sept. 18th when I go to see him. Have also had some hip pain but not real bad. Worried myself to death about multiple myeloma but my primary doctor has run all kind of tests to rule that out. Hopefully Rheumy will be able to give me something gentle to take as I have low kidney function.
Oh yes. I have pain in my ribcage, every time I breathe. I did not know there was a word for it.
yes. Definitely. My Rheumatologist diagnost it. I have had RA for over 30 years now needless to say I have had my share of pain. But nothing as bad as this. For the first time I actually sat in the doctor’s office and cried because the pain was so bad from the vibration of the car getting to the office. the doctor prescribe a combination of gabapentin and Cymbalta. The pain was almost gone overnight. I stayed on the medication for some time mostly out of fear that should I discontinue the meds for the pain would return.if your doctors do not believe you please ask them to do a little research and consider prescribing medications for you. They were truly a magic combination of pills.
I too have suffered with this and yes, I ended up in the ER the first time when it happened (this was pre RA diagnosis) and was told I had pluresy. The second time I was at work and my boss had a coworker drive me to the ER. This time there was no explaination. Both my rheumy and GP have diagnosed this as costochondritis. It is very scary to go through, and you do worry that it may be your heart as we do know that RAD can effect your heart. I am glad to see I am not the only one suffering through this painful condition. This is why I am so glad to have found RW- you have made me feel like I am not alone and not crazy about some of the mystery pains! Thanks for all of your hard work.
God bless us all!
I have also had past episodes of sore ribs that last for months at a time. When I had an upper abdominal CT they discovered I has several 5-6mm lung nodules . They were checked at 7 months and were stable so I am very blessed , it was scary because my sister died of lung cancer. People don’t realize how many complications RA cause. This site is very helpful because I really don’t have anyone who really understands the disease to talk to. I have always had to take care of my husband due to his back problems were he would get episodes that put him in bed for weeks at a time and even though I was having flare ups I would have to take care of him plusb work 8 hour days . I do know my husband loves me but always has something going on with himself to help me.
Thank you for posting this!
I have inflammatory arthritis and have been getting this chest pain for almost an year now. Neither my rheumy or my GP are too concerned about it since I am taking Celebrex everyday to cope with inflammation.
But yeah it still hurts and there are times when I want to go to the Accident and Emergency to get it checked out but I do not want to waste anyone’s time.
I was stunned when I saw this post about costochondritis. I was diagnosed with this back in 2007-2008 by a heart doctor and now in a few weeks I will be going to see a rheumatologist for other symptoms related to RA. I’m in denial, SERIOUS DENIAL that I have RA. It’s taking a physical therapist and a sports doctor to tell me that there is a huge possibility that I have RA. I have been fighting for years to find out why I hurt and ache and I actually was told to my face that I was depressed and it was all in my head. Someone at my job actually approached me and told me that she was thinking of me and that she has RA and if I needed to talk, she was there. I felt better. I’m just scared I guess because I have a family to take care of. I think I’ll stick around and keep myself informed.
Thanks for “listening.”
My husband has suffered with RA for 15 years. He started having severe chest pain and tenderness. We went to the hospital ER and they pretty much gave him a bandaid and sent him home. 3 days later the chest pain was worse and we went to a different hospital. They did “tests” and said to go see a pain management doctor. I like to do research and I entered his symptoms and found this FANTASTIC website. So I know now that there is hope for him out there! Thank you so much. I have made my notes to take to the RA doctor and pray they can help!
Thank you for this post. My spouse read it first and immediately shared it with me because this is one of my most painful sites with RA. My rheumatologist has decided initially that my specific diagnosis is ankylosing spondylitis and possibly Sjogren’s too. And he, thankfully, recognized the costcochondritis as a symptom of my condition. I, too, have spent time in ER spinning wheels, nervous, and anxious as to whether I was really having a heart attack; even though I felt fairly certain it was in between my ribs at the site of the joints.
Mostly I am grateful simply to have someone with arthritis confirm that they, too, experience this. A person can think they are crazy when all the symptoms start adding up, especially when folks tend to act mystified by the description. All the literature, written in technically appropriate medical style does not come close to actually describing what this disease/condition is like to experience.
We are bookmarking your site and will keep up with the posts! Again, we are sincerely grateful to learn of your supportive shares/posts.
Many blessings. js
Well Im now 100% sure I do have RD, seronegative results and all. I too have had these Costochondritis pain since I was in my late teens. The pain was so bad, like a knife was stabbing me in the heart each time. Id take a breath and the pain would stab me again putting me on my knees. Saw a family doc and they diagnosed it as Acid reflex. Now I know its not, as I still get this pain, but its not as severe as it used to be. Its def painful, and i have a hard time catching my breath, while my heart palpatates erratically. My recent doc is the only one that knows I have this, but he didnt give it a name. I told him, i thought i was having heart failure, and told him this. But still he doubts that i have RD. Can this actually proves to him, that this is RD?
My RA doctor swears that there are no joints in the ribs so my pain cannot possibly be related to RA, hence it must be fibromyalgia or a figment of my imagination. So, why is there noticeable swelling along the ridge of floating ribs? Why is it hard to take
Yes I have suffered many times from costralchondritis and my Rhuemie is very familiar with. At first he tried treating it with Indocin but it was not successful. Then we tried a topical anti inflammatory lotion, again unsuccessful and the pain is increasing. It went down both sides of my sternum and included the entire sternum being painful but particularly the ziphoid process which is the triangular notch at the bottom of the sternum. One day the pain was so incredibly intense with an extremely quick onset that I went to the ER and was worked up for cardiac complication and kept for a 24 hour observation and a cardiac stress test. Although I told each cardiologist about my difficulties with RA (and no I do not have gnarled or crippled hands so they sort of blew that diagnosis off). I am convinced that if you go to the ER for an RA complication you are SOL because nobody takes it seriously and nobody knows how to treat it….it is a huge bill and a huge waste of time. I left and went to my Rheumies office and he diagnosed Tietze and gave me 24 injections into my sternum and ribs over three days of lidocaine and prednisone and then prescribed Lidocaine Patches to apply 12 hours on 12hours off. It took awhile but finally resolved. Even when I went back to work at the same hospital that I was treated and encountered some of the same docs they inquired how I was doing….when I told them about the Tietze and the injections they just sort of looked at me as if I was explaining some sort of voodoo medicine “that made the little lady happy that she got a diagnosis and a treatment” whatever! I’m just thankful that I have a highly educated Rheumatologist that knows how to treat me and despite nothing working after 9 years of this disease….he refuses to give up on me. God love him!
Hello Everyone, I too have costochondritis fortunately at the moment it is not severe but each breath is affected. I am fortunate that my physician is very aware of the many “possible” presentations of RA and is willing to treat (costochondritis with injections if I am willing) etc. The biggest comment I would like to make is that although our symptoms are often “just” (said with great sarcasm)related to the RA such as costochondritis it MIGHT be your heart sometime. In medical circles we say that “people die all the time of indigestion” meaning they think they once again or newly have indigestion take antacids and die; when actually they are having a heart attack. So, please be pragmatic, do not always assume a benign reason for the chest pain. Cardiologists are mostly aware of costochondritis however they must practice defensively to save lives. We are in a very tough position, ourselves confused by our symptoms, cut yourself some slack, pursue treatment and pain relief.
Hi Kelly, thanks for this post. Wish I had read it before I ended up in the emergency room on New Year Eve for chest pains. The up side is I have an even greater appreciation for emergency medical staff. They tested for everything, decided that the only problem they could find was a bacterial infection in my urinary track and sent me home. Please keep these great posts coming. Thanks again.
I have had RA for 9 years and was recently diagnosed with Chronic Myloid Leukemia- (which they tell me is no way related to the biologics that I have taken for so many years) But to treat the leukemia, they had to remove me from all RA meds except for prednisone. Well, the medicine they put me on has horrible lung side effects like pulmonary embolisms and pleural effusion and shortness of breath. After 6 weeks on this medicine, I developed the shortness of breath and pain in my ribs-more my lower ribs than my upper ribs or sternum. And I automatically thought it was the medicine. They actually have taken me off the medicine and my primary doctor thinkis it may be asthma related to the medicine. I never thought about the RA. It would make sense though. It is rearing it’s ugly vile head everywhere else in my body. why not show up somewhere new?? Thanks for making me think outside of my new box!!
Sarah, just wanted to say that I am sorry about the Leukemia. Sometimes it feels like another thing is piled on top of the last. I know treatment is a huge hurdle, but girlfriend, if you can “do” RA you can “do” leukemia!! God Bless your journey.
My rheumy has tossed me over to my pulmonologist and cardiologist, after a miserable summer. I did pulmonary function tests, my lungs are at 54% capacity. Twice a day I nebulize meds, Brovana and budesonide. I also use Spiriva & Singulair. A high resolution CT scan showed no damage, so on to the cardio. Pulm. doc insisted on a heart catherization , both left & right sides. I am scheduled for that on Fri. 10/18. This will be my 5th cath 🙁 Costochondritis was never in the picture…this is getting old fast… as am I!
Good luck on Friday Lois.
Rib pain, unbenounced to me, was likely one of the first major signs of my RD journey. A year before my official diagnosis I was sitting in urgent care with severe chest pains on my left side. They ran a full cardiac workup and declared “anxiety” as the cause despite my lack of actual anxiety as a trigger. I knew that was not answer and quietly suffered with the pain. The only positive moment back then was knowing that my heart was OK and the pain may be something else. When I finally started getting “trademark” RD symptoms did all the pieces of the puzzle start fall together. I still suffer with rib pain along with the myriad of other pains through my body. All I can do now is try to pay attention for if the pain changes. Its no wonder RD folks are more likely to ignore more serious cardiac issue signs. When your always in pain, more pain is just another day like yesterday.
Chest pain plagued me for years. Two years ago, I ended up in ER three times within a few months thinking, like many of you, that I was having a heart attack. Paramedics were called; no heart problems. I just could hardly breathe the pain was so bad. The third time I had severe pain my husband drove me to the hospital 25 miles away because it was better than others nearby. I was admitted for tests as they also found it was not related to my heart. Two days and many tests later, I met a rheumatologist (who is now my practitioner), who diagnosed me with pleurisy–an infection between the lining of your lungs. Sure enough with high dosage of antibiotics, the pain began to dissipate, but not before I had spent 6 nights in the hospital–the longest in my life. Horrible pain, don’t want to experience that again thank you. Good luck and good living to all of you.