3 Topics in the News on Rheumatoid Arthritis Heart Disease
Rheumatoid “Arthritis” in the heart – no joints, but plenty of problems
Often, I have sharp chest pains, but I know it’s not my heart – click here if you don’t know what it is. (Hint: there are joints along the sternum.) But when a large butterfly flutters in my chest and tries to escape through my neck, I know that IS my heart. For a while I’ve also had shortness of breath upon exertion (with exertion being taking a shower).
Somehow with my mostly normal-looking hands, I thought I might escape other types of Rheumatoid damage. I know better, so maybe it’s wishful thinking. Or maybe it’s the docs who’ve told me I didn’t look sick, and paid no attention to my fevers, permanently swollen knees, bent toes, and deteriorating spine. For whatever reason, I’m facing reality that I’m not exempt from the high risk of atrial fibrillation in RD. So, as I make my appointment for a heart ultrasound today, let’s look at 3 things from my long list of Rheumatoid / heart news items.

1) Rheumatoid disease changes the left ventricle of the heart
Researchers at Mayo Clinic found that Rheumatoid disease is strongly associated with abnormal concentric remodeling of the left ventricle of the heart.[1] The investigators determined that “RA disease–related factors may promote changes” in the geometry of the left ventricle of the heart. The association was not attributable to traditional cardiovascular risk factors and comorbidities. (In other words, they necessarily can’t blame your weight, smoking history, or the fact you’re not a vegan. It’s the RD.)
By the way, Myasoedova et al. are not the first to recognize a problem with the left ventricle in Rheumatoid Disease. Bhatia et al. raised an interesting question in 2006: Left Ventricular Systolic Dysfunction in Rheumatoid Disease: An Unrecognized Burden? Seven years later, it is still largely unrecognized, but I’m glad to report that a handful of doctors are investigating it.
2) They’re debating whether evidence warrants cardiovascular risk management in PRD
This summer, a debate continued about whether “evidence supports” the management of cardiovascular (CV) risk in people with Rheumatoid Disease (PRD).[2] This argument takes place at the intersection of science and management of resources. The question isn’t whether PRD have increased CV risk, but how much or what to do about that. In 2010, the European League against Rheumatism (EULAR) had published 10 recommendations for cardiovascular risk management in PRD.[3]
One thing stands out as this debate continues, few have recognized the reality of recommendation number one: “RA should be regarded as a condition associated with higher risk for CV disease.”[3] Reading up on atrial fibrillation today as I made my ultrasound appointment, one medical site after another gave a list of those at increased risk for “a Fib,” stroke, or other CV disease. You guessed it: none of them listed RD as a risk factor.
An article by Nathan Wei appearing on several sites states: “The notion that RA is a potentially crippling disorder is widely accepted. However what is not generally known is that it is a potentially lethal disease leading to an increased risk of heart attack and stroke.” He discusses a report that heart attack risk is lessened with TNF inhibitor (Biologic) treatment.
3) Higher prevalence of diastolic dysfunction in Rheumatoid Disease
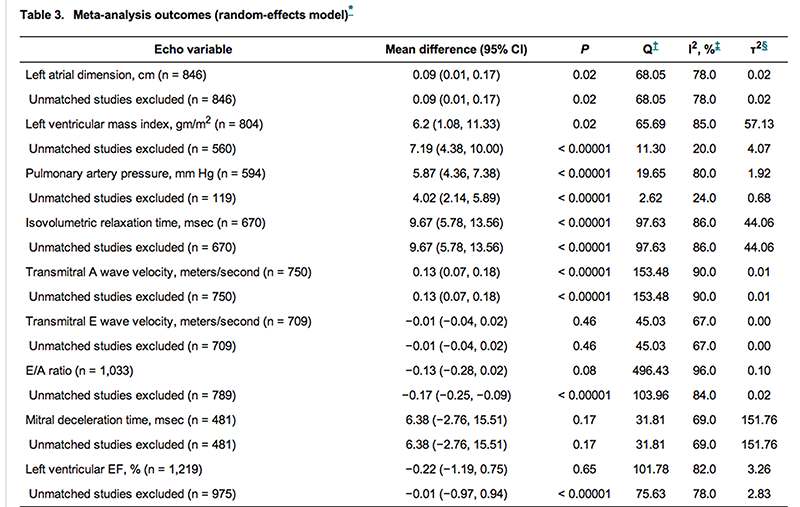 Aslam et al. conducted a literature review of 25 studies of PRD to determine whether diastolic dysfunction and other cardiac parameters were different with RD.[4] They found “Patients with RA were more likely to have echocardiographic parameters of diastolic dysfunction, and have higher systolic pulmonary artery pressures and larger left atrial sizes.” The screenshot shows part of Table 3 of an analysis of outcomes.
Aslam et al. conducted a literature review of 25 studies of PRD to determine whether diastolic dysfunction and other cardiac parameters were different with RD.[4] They found “Patients with RA were more likely to have echocardiographic parameters of diastolic dysfunction, and have higher systolic pulmonary artery pressures and larger left atrial sizes.” The screenshot shows part of Table 3 of an analysis of outcomes.
HAVE A HEART
So what? Every few months we come back to this topic of Rheumatoid heart disease for two main reasons:
1) There’s a lot to be learned.
2) It’s the systemic effects of RD that make us feel unwell and shorten our lifespans, not twisted fingers.
This post does not begin to cover the ways that Rheumatoid Disease affects the heart. It would take a whole book to do that topic justice. There is a section on the heart in my first book, and meanwhile there are 18 posts on this site on the effect of RD on the heart – click here to read. Our mission is to get the best care we can for ourselves and the patients we care for, AND to help the medical world understand the ways RD affects patients.
MORE: Want to know more or know a doc who doubts the CV effects of RD? I recommend this short article written by a doc who leads the Preventive Cardio-Rheuma Clinic at Diakonhjemmet Hospital in Norway: RA and Carotid Plaques: Five Things to Know.[5] It reads much like a blog on this site with a list of quick facts and footnotes.
Recommended reading
- Rheumatoid (Arthritis) Heart Disease
- 20 Facts About Rheumatoid Heart Disease
- Why Rheumatoid Disease Patients Still Fall through the Cracks
- What Would the Car Mechanic Say If You Didn’t Look Sick?
- RA News Vol. 8: Predicting TNF Response, Prednisone Increases Remission, New Mayo Clinic Heart Disease Risk Study
FOOTNOTES




Another great posting Kelly, I’m going to make a copy and make sure my rheum reads it as he doesn’t seem too concerned about my issue when it comes to CV questions. However my wonderful GP is and when I first saw her last year, she immediately changed the HBP med to one that didn’t work in my pancreas as many do (leading to diabetes) and then gave me a EKG and sent me for an cardio ultrasound. No changes yet which was good, but still unexplained why my pulse goes sky high without medication for that. I feel confident she is keeping an eye on it. One question I always seem to come back to is it the RD or the meds? I believe its the RD but she had some suspicion the MTX and or combo with biologic may attribute some to the crazy pulse. I will be giving her a copy of this too.
Thanks again for doing all the research for us and putting it together for us. Good luck with your ultrasound!
xo
Wow, how appropriate you should publish this today!!! That butterfly has been in my chest for a few years, before I was diagnosed, and lately he has been around a lot more. I have high blood pressure when I never did before my RD diagnosis, and I get winded going up a flight of stairs. I am not even 50, and I am not overweight or otherwise not well! My father had Afib issues, so I have known for months that this is something that needs to be addressed soon. I am going to my rheumatologist in two days, I am sure he will send me to PCP, but either way it’s a issue that I need to deal with. Thanks for reinforcing something I already knew, and giving me that little “push” Kelly to do something about it. I hope your tests give you some positive news!
I am floored. This blog has been hands down the best source of information for me regarding my RA, but nothing prepared me for this article. My jaw literally dropped open. I have had symptoms of RA (undiagnosed as such) since childhood. I am also seronegative, which brings all kinds of skepticism to the table when dealing with rheumatologists. When I was 30 and in the best shape of my life, I had an episode of pleurisy that landed me in the ER. At the time the docs took scans and X-rays. At a follow up with my GP, he asked, “Did you know that the left side of your heart is flat?” That was as far as it went. Now 10 years later, I read this and, although it’s not good news, felt some hope of achieving some medically validation.
Thank you so much for all you do.
I am -unfortunately -living proof that RA causes cardiac problems. I had no evidence of any cardiac disease until two years ago. I started noticing that “butterfly” feeling, then big runs of tachycardia (rapid heart beat), finally swollen ankles and marked shortness of breath (SOB) and ended up in emergency. Round one: ten days in hospital (large pericardial effusion and mitral prolapse). Round two: a week in hospital on a cardiac unit. Round 3: same cardiac unit but then I had surgery to open up the pericardium to allow it to drain. Three lengthy recoveries.
Right now, my heart seems good. But I will probably be followed by a cardiologist the rest of my life.
(Female, fifty, severe RA x 20 years now). My GP still thinks that RA gives you some sort of shield against cardiac problems, but that seems to be pretty old school thinking based on the latest evidence.
Thanks, Kelly for another well written article.
how OLD is that “old school”? my grandfather and HIS grandmother both succumbed to it — I think that GP actually is believing some mythical wives tale. 😉
Seriously, thanks for sharing Christine. I hope your docs take good care of you.
Cardiac disease is a serious issue for us. If we relied on our rheumatologists for complete info, we would all be in big trouble. I had ‘explosive onset’ RD at age 40. My rheumy was GREAT, and he sent me to a cardiologist even though I had no symptoms, but he knew the risk and sent me anyway. I had an abnormal EKG showing extensive scarring along the anterior wall of my heart, a result of previous ‘silent’ heart attacks. Now that I have moved to Florida, I asked my new rheumy for a copy of my recent bloodwork to give to my cardiologist since I had an appointment coming up, and my new rheumy asked me why I had a cardiologist. (I got a blank stare when I answered ‘because I have rheumatoid arthritis’) It would be nice for once to have the ‘specialists’ teach us something instead of the other way around. Very discouraging.
great point Elaine. Thanks for sharing. I had a similar discussion yesterday with Donna.
I agree with you. Btw, it is not a rheum doc who is sending me for the ultrasound. The last one I saw knows less than my kids about this disease – didn’t recognize the vasculitis or examine my joints… https://www.rawarrior.com/keeper-or-loser-im-not-giving-up-but-what-do-you-think/
Kelly, thank you for your research and all the time and effort you put in to sharing this information. I am grateful to God for the knowledge you share. My RD is progressing and I have had the sternum pains for years. Tomorrow I am seeing a dentist for investigate RD-caused TMD (TMJ disorder), because my right TMJ has been causing severe pain as well as stimulating nerves that essentially gives me two or three severe toothaches simultaneously. Of course my rheumy isn’t at all interested. More ibuprofen and gastritis, thank you. But I never would have thought to link the chest pains and TMD to the RD without your work. Thank you. Let us know how the US turns out, please.
thanks Tom. good luck.
I am 38 and have been diagnosed with RA for 5 + years. I had no heart issues until I started to notice my blook pressure slowly creeping up over the past year. My prevous rheumy did nothing. he left and I am being followed by a much younger rheumy. I finally went to my PCP for HTN meds. When I asked by rheumy to prescribe them (as I firmly believe it is caused by my RA) she would not. However she noticed my tachycardia and suggested I see a cardiologist. I went and ended up being diagnosed with prolonged QT intervals. New medications to reduce HTN and heart rate. Within a month I was in the ER with an episode of supraventricular tachycardia where my heart rate was at 200+ for 90 minutes. I am now having a cardiac ablation to keep it from happening again as they cannot do anything else since I was already taking the medication when it happened. RA seriously affects our other systems. My rheumy is good but we have to ask for what we need as well. No one else noticed by HTN until I said something. I get rituxan infusaion every 6 months- due tomorrow. Thank you Kelly for all you do. You have helped me and I also sent my mother to this website to better understand this illness. It has helped her too.
Thank you, Kelly, for the validation. I have said for the last 4 years that it was the RD that caused my dad’s massive heart attack and killed him. No one would believe me they kept telling me it was the MTX. Before I was diagnosed in June of 2010 I kept telling my family I was dying did not know if it was my heart or if I had cancer but I was dying. Come to find out I had RD. I also get short of breath and have dull pains in my chest sometimes. But according to my Rheumy and NP everything looks good on all my heart test so far. Kind of scary though that is what they told my dad 4 months before his death “looks good, you have the heart of a 40 year old man. ” He was 67. Four months later he was on a vent and 5 days later we took him off and he passed within four minutes of being unhooked.
No one has a clue to what this horrible disease will do to you. I hate getting the “Oh yea, I have that to in my neck or back. ” I just look at them and say ” Really, what kind of chemo do you take?” You should see the look on their face when I say that.
Good article I have found this information in various places like the summary.my Dr knows but many health care professials do not
I’m having this issue of pre-atrial fib signal disruption. I also have some other heart issues my PCP has detected. I first learned of the signal issue when I had an EKG prior to my a total knee replacement.
I’m going to send a link to this blog to my PCP. He and I are new to each other since I re-located last June. I know he has hit the books on MTX and RA. He is all over this cardiac stuff I’m developing. I’m quite lucky to have found him.