New Criteria for Rheumatoid Arthritis
 New criteria for studying Rheumatoid Arthritis
New criteria for studying Rheumatoid Arthritis
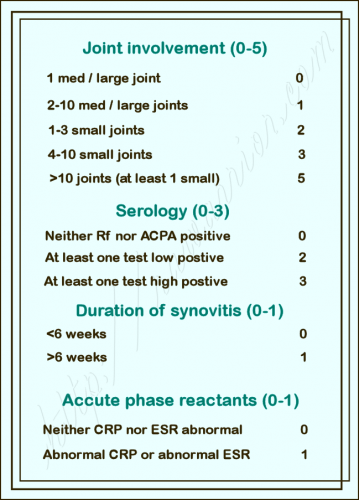
Last October at their convention, the American College of Rheumatology unveiled the revised criteria for classification of Rheumatoid Arthritis (for more detail on how the point system works, please click that link). This month, in coordination with the European League Against Rheumatism (EULAR), they have announced that the new guidelines have been adopted in the September issue of Arthritis & Rheumatism. The final criteria seem to be equal to what was revealed last fall, with some additional wording.
As in the past, the criteria are technically created to be guidelines for the clinical classification of Rheumatoid Arthritis, especially for researchers and clinical trials. However, since IRL clinicians need some guidance too, the new criteria will be used in practice for diagnosis, just as the old ones were – at least until there is an alternative. It seems the criteria are of particular interest to insurance companies and governments who manage healthcare as well.
What’s next with new criteria for Rheumatoid Arthritis?
The next step is to create the first actual guidelines for diagnosis of Rheumatoid Arthritis. According to Laurie Barclay, MD for Medscape, the creators of the Rheumatoid Arthritis criteria “hope that development of this new set of classification criteria will further accelerate RA research. Dr. Hawker suggests that the next logical step should be to use these classification criteria to develop diagnostic criteria for RA, which could be used in rheumatology practice.” I also read some comments expressing concern that non-rheumatologists may be considered less equipped to use the guidelines. Perhaps new diagnostic guidance could also include some indicators for general physicians or for referral to rheumatologists. Let’s hope so.
Why do we need new criteria for Rheumatoid Arthritis?
The hope of everyone is that the new guidelines will increase treatment of Rheumatoid Arthritis by helping more patients to be identified earlier and receive coverage for the appropriate treatment. The 1987 ACR guidelines for Rheumatoid Arthritis were a description of later stage disease, as many now admit. “This new classification system redefines the current paradigm of RA by focusing on features at earlier stages of disease that are associated with persistent and/or erosive disease, rather than defining the disease by its late-stage features. This will refocus attention on the important need for earlier diagnosis and institution of effective disease-suppressing therapy to prevent or minimize the occurrence of the undesirable sequelae that currently comprise the paradigm underlying the disease construct ‘rheumatoid arthritis.’”
“Minimize the occurrence of the undesirable sequelae”? Did he mean “treat RA sooner so fewer of us need wheelchairs or joint replacements”? I thought so.
Many doctors have been practicing for years “outside” the guidelines by treating patients who obviously have Rheumatoid Arthritis, even though they do not present with RA that seems to fit the typical old conception. Some patients have been thanking God there are some doctors like this. However, other patients have gone untreated for years, suffering much damage, as many of you know too well. Here is what an ACR doctor said last fall when the new guidelines for Rheumatoid Arthritis were first revealed:
The new criteria “mirror what we are doing in practice, or what we think should be done in practice,” said Dr. Eric M. Ruderman, a rheumatologist at Northwestern University in Chicago who was not involved in creating the new criteria.
“At Northwestern, most of these patients are getting treated, but I’m not sure what goes on in the community,” Dr. Ruderman said in an interview. “The leading edge says ‘treat all patients who meet the new criteria.’ Will the rest of rheumatology follow that? It would probably have happened anyway, but [the new criteria] may help drive that” more quickly.
“We have patients with persistent, inflammatory arthritis who do not meet the current classification criteria but have persistent and functionally disabling disease. [The new criteria] set the stage for us to treat patients earlier,” said Dr. Weinblatt, professor of medicine at Harvard Medical School and codirector of clinical rheumatology at Brigham and Women’s Hospital, both in Boston. The new criteria “will allow more rapid institution of disease-modifying therapy.”
Editd 6/11/11: replace broken link.
Recommended: Details about why the changes are needed & what they mean:
- American College of Rheumatology Redefines Rheumatoid Arthritis
- American College of Rheumatology Redefines Rheumatoid Arthritis, Part 2
- American College of Rheumatology Redefines Rheumatoid Arthritis, Part 3
How would YOU describe classic RA? What about Classic Rheumatoid Arthritis?



I fully support new guidelines that would help any doctor properly diagnose a patient with RA early on. My GP improperly diagnosed me with synovitis (no blood tests ordered) and had me on Aleve for a year before I switched doctors and discovered I had RA. I would like to think my damage would not be as severe as it is now had I been properly diagnosed.
How is the scoring added up? I just don’t get how 2-10 med/large joints is worth 1 point while 1-3 small joints is worth 2 points.
Yes, that is perceptive. I think it is a reflection of the original bias toward *hands* in diagnosis. It’s a big improvement because small bones could also be feet now. Many of us started with feet — & had hands affected much later. That tends to delay diagnosis, too. Hands are almost always affected, but for many it’s much later on.
btw: That doesn’t mean I agree with it – we probably both know plenty of patients who had larger joints affected first.
That sounds so “dumb” about your synovitis diagosis since that is a main symptom of RA. What on earth did that guy think was causing that persistant synovitis? An Aleve deficiency? Sorry, it’s late so I’m a bit punchy. 😛
I know … looking back now, I don’t know why it took me almost a full year before switching GP’s. The new one that I went to suspected and had blood work done on my first visit to him. I guess my first GP skipped a lot of classes at med school. BTW, I loved the Aleve deficiency. lol
Bottom line, we all need to question our doctors when something may not sound right or isn’t getting better. Doctors make mistakes too and, as in my case with my first GP, I trusted him completely.
Oh, that is so true. A lesson we learn the hard way sometimes. Did you see the e-patient book yet? (link on the menu) This is exactly the point of it – patients being part of finding answers.
I score high enough, but the first and most troublesome symptoms for me were the low grade fevers, fatigue and the morning stiffness. I didn’t even think the hand pain was a big deal at the time – I mean, sure, they hurt and swelled – I just thought that was my age catching up on me. I’ve had the fevers, fatigue and stiffness for two, two and a half years now. I think if those items where on the list, I might have achieved a diagnosis sooner than just a month ago. My ACPA test was strongly positive, so clearly my bodies been playing host to RA for a while now.
Practically any change in diagnostic criteria is welcome, but clearly there is still significant hesitance within the medical community to weigh anecdotal input from the patient. To paraphrase Bill Clinton, “It’s the (PAIN, FATIGUE, MALAISE, BRAIN FOG, etc.), stupid!” Truly … how many people do we believe fake RA so they could can take chemicals that have miserable side-effects and damage your organs? Even those who max out on magic diagnostic points are finding it more & more unlikely to receive narcotics, so it can’t be that … like I’m going to go from doctor to doctor seeking a prescription for Motrin or Prednisone? I’d laugh, but it hurts my shoulders. After a lovely 3-week steroid honeymoon after shots for rampant poison ivy, I’m having the old pain & stiffness, plus new pain & stiffness. And it’s making me mad! So, I’m planning a showdown with my GP this week, and I’ll be taking this post with me – thanks, Kelly.
Jackie, I’d love to hear about how it goes! I’m mad at RA too right now. I put my hands into warm water to wash them and omg the seconds of relief. Then, I can say, HOW MUCH they were hurting & I wasn’t even admitting it. I put it out of my mind until there was a moment of relief and it all was right there. I’m so tired of feeling like I have 15 broken bones and I can’t walk another step if my life depends on it!
Back to your fantastic comment: that is so well stated!! This is what we MUST do tho. There is not other way to treat an invisible disease that does not show well on tests. Hello?? :heart:
Acheyness in the morning especially if i sit for more than a few minutes and now it sometimes continues all day, my experience with prednisone has been curious, 10mg of it and the pain is gone within an hour, 5mg it only drops the level from a 6-8 to 2-4 but by afternoon its dropped to 2 or less.
im now taking 5mg in the am until i can see my RA doctor this week for advice and hopefully some sort of treatment, will he keep me on it with low dosage? I don’t know time will tell.
Maybe the low dos will be continued & another medication added? Let us know how you do. Good luck.
Although it is little difficult to memorize these criteria for daily practice, but it more beneficial and detects a lot of missed cases.
Thanks for you
I have fatigue, low grade fever, joint pain, Swelling,excessive sweating, problems gripping/dropping, creaking joints and nausea. My GP did an anti-ccp test on me several months ago and it was negative. My symptoms have since worsened and she sent me to a rheumatologist. It took me 4 months to get in and when I saw him he said I “probably” had Ankolosing Spondylitis (sp?), plus Fibro, plus carpal tunnel. I have had MRIs and Xrays in the last yr and AS is not possible according to my dr. So now I am back to no diagnosis and completely miserable. It has been a year now….any ideas??