Prednisone Versus Prednisolone: the Same for Everyone?
Whether medicine is personalized or not, patients are
 It’s fascinating how drugs are metabolized differently in different people, with different side effects and varying levels of benefit. But, prednisone is one thing we hear works the same on everyone. Is that right?
It’s fascinating how drugs are metabolized differently in different people, with different side effects and varying levels of benefit. But, prednisone is one thing we hear works the same on everyone. Is that right?
Prednisone works well enough on most Rheumatoid patients that it’s used by some doctors as a method for diagnosis: response = Rheumatoid Arthritis diagnosis. But, occasionally, patients mention that prednisone does not work as well for them. Some say that they need a high enough dose to be effective that the side effects are not worthwhile. Others say it just doesn’t work. And there was a fascinating comment recently by Belinda about prednisone working differently than prednisolone in some patients.
Prednisone works for everyone: FALSE
Three years ago, I stumbled upon a statement about the effectiveness of cortisone that jumped out at me. It was a historical article about the invention and early experimentation on Rheumatoid Arthritis and cortisone, which is of course much stronger than the prednisone prescribed today. At what we’d today consider a preposterously high dose, Dr. Ward at Mayo Clinic treated the first 100 patients with cortisone. Think of it as an early clinical trial. Their findings? Lots of side effects and an “effective response was seen in all but one patient.”
Stunning. Even at that high dose, they found one non-responder to prednisone.
After Belinda’s comment, I started thinking about this again. I wonder how many non-responders to prednisone there are. And why doesn’t it work for them? Would prednisolone work better, as it seemed to for her?
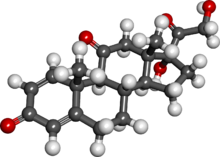 Katie Beth and I studied the Wikipedia diagrams the other night. She’s studying microbiology and organic chemistry right now so she was a big help. The prednisolone has two more hydrogen atoms on the molecule than the prednisone.
Katie Beth and I studied the Wikipedia diagrams the other night. She’s studying microbiology and organic chemistry right now so she was a big help. The prednisolone has two more hydrogen atoms on the molecule than the prednisone.
It reminds me of T-3 and T-4. I’ve had thyroid disease since age 15 and this is a simple, but critical truth that is still being learned by many in endocrinology: some patients do well on levothyroxine supplementation (T-4). Other people do not as readily convert synthetic T-4 into the active form, T-3. The tiny difference of one atom on the molecule makes a difference so that while T-4 lowers TSH and improves blood results, some low thyroid symptoms remain. The solution? Some patients need to add supplementation of T-3.
I wonder if the comparison is a plausible reason for the difference in the way prednisone and prednisolone work differently in some people. Either is obviously rationale for a more personalized approach to medicine.
Early on, cortisone was called either magic asbestos to protect patients from inflammation or a fire hose to put out inflammatory fire. Maybe it’s more like something that can throw a switch in the body to turn off inflammation – it’s just that not every person has the exact same access to the switch.
What’s your experience with prednisone or prednisolone?
- What dose of prednisone do you have to take before it works for you?
- Are there too many side effects at that level?
- Do you know whether prednisolone works differently for you?
- Is there anyone who does not respond at all to prednisone?




I have been living with RA for five years. Prednisone has been the only thing that works for me. When I have a flare, it can take up to two days to hear back from my physician. I have a history of increasing my dosage during these times which really upsets my physician. They want me to sit in excruciating pain and miss work while I wait to hear back from them. I am currently on 10 mg per day and I have tried to decrease my dosage slowly although I just end up in a flare up. There is such a disconnect with my physician, if he can’t see swelling and inflammation he does not believe it is my RA.
thank you kelly once again! i am currently on long term -2.5- 7.5 mg prednisone and it works well. i have some bone-mass loss and weight gain and perhaps my periodic nights of sleeplessness are due to the pred. Otherwise, it helps me in transitional phases between the “real” meds. i hope to wean down to 2.5 in a month and then perhaps go off altogether. it’s a game of risk benefit – the short term benefits are fabulous – the long term are to be seen……i will ask my rheumys at mayo about the other steroid – it hasn’t come up.
I have never been on Prednislone and am now off Prednisone. I will never take it again! It made my skin so thin that whenever I bumped into something sharp it caused my skin to tear. Even a chair with somewhat of an edge would do that. I have several scars from that happening. It also caused big red spots under the skin on my hands and arms that would go away and move somewhere else and leave brown spots that I still have.
Kay, if you don’t mind saying, how long did you take it?
I am a huge fan of prednisone. I have been on prednisone for almost 2 years now. I am currently on 2.5mg/day and prednisone works for most of my symptoms. Before I was diagnosed with RA, I was put on 10mg a day (which then became 15). I had difficulty (flare-ups) in being reduced to 7.5, then 5 mg/day before also getting on methotrexate. The only bad thing is the weight gain (always STARVING) and that I still have stiffness/deformity/swelling in my right thumb and finger right next to it, but I am able to walk and get in and out of a chair (which was becoming increasingly difficult prior to prednisone). I have more side effects from methotrexate for about 48 hours after taking (naucious/overheated/irritable), but my joints also feel better with methotrexate.
I’ve had RA since the birth of my first child in 1992. I have been on everything from Advil, to Naprosyn, to Methotrexate, to Plaquenil, to Prednisone, to Embril…… the list goes on. I am presently injecting with Humira every two weeks and taking 5-6mg of Medrol daily. I still have some inflammation but am in pretty good shape – no major flares in several years – but as always, waiting for the shoe to drop. I have been using a steroid daily for at least 18 years. Use of steroids requires strict management of my immunities and knowing how my body feels at all times. I am now 52, functional, no joint replacements yet, and not overweight (weight management is CRITICAL!) Together we must fight this dreadful disease!
After my diagnosis at age 7 I was never on anything aside from ibuprofen and naproxen. It was not until after a mega-flare after having my son that I was ever given either prednisone or a DMARD. At that time, the risks of DMARDs outweighed the potential benefits for someone who only had a “mild” case of sero-negative JRA. Sadly, I now pay the price for that lack of treatment in that I have a good bit of erosion, deformities and joint damage. Because my labs have always been fairly good, my doctors have a hard time figuring out whether my RA is active or whether I am just dealing with prior damage.
I cannot say whether I do better with prednisone vs prednisolone because as far as I know I’ve not had prednisolone. But I DO know that I react better to some corticosteroids than others. With my previous two RDs, they used Decadron (dexamethasone) for both intra-articular and systemic injections. There was no problem with them doing that with my then insurance company.
When I was at the nursing home, I was in a major flare and asked my dr for a systemic injection. I would loved to have had a couple specific joints injected too but I didn’t think he would do an intra-articular one and would send me to either an ortho or an RD and at the time, the pain of being transferred would have outweighed the benefit of the joint injection because this was when I was still being transferred by ambulance because my knees didn’t have the range of motion to allow me to sit in the seat of a car. As was normal for that dr, he asked me what I’d had in the past and what worked best for me. He was really great about listening to me when I said what worked and what didn’t. I told him that from 2006 on I’d had nothing but Decadron that I knew of and it worked well, except for the occasional headache afterward. But that I could tolerate the headache to get the relief the shot gave. I think my RD gave me 4-8mg depending on the situation. If it was a shot given prior to me doing something that we knew would send me into a flare, like going on vacation, etc. I believe he would give me the 4mg but if it was a flare that had been ongoing, he’d give me 8mg. I know the RD he worked with had given me what she called a “double dose” in the past b/c of the severity of my flare. So my doc at the nursing home wrote the script, the nurses ordered the shot, gave it and I felt better. Then a few weeks later I got a letter from my Medicare Part D insurance co. They don’t cover Decadron, so they had denied the claim. It wasn’t a HUGE deal but it was a hassle. I knew that we could appeal and have the paperwork filled out to show it was needed and get an exception but I did NOT want to have to do that every time I needed a shot, because I knew the nurses were overworked at the time and filling out paperwork for me to get an exception was too time consuming. At that time I was getting them every 2-3 mo because I’d not re-started oral pred daily. So, I asked what they did cover. Their answer was Medrol (methylprednisolone). So I told my doc that was what I needed. I am unsure of the dose he gave me but I can say that I went from needing a systemic shot every 2-3 months to barely feeling any relief which did not last more than a few weeks and at one time only 3 wks passed before I was miserable and begging for another shot. And this is despite having fairly good pain management meds. In fact, he’d upped my pain meds from: 10mg methadone scheduled three times a day with hydrocodone 750 PRN three times a day to 15mg methadone scheduled four times a day and another 5mg PRN three times. It took my total daily dose from 30mg methadone to 60-75mg a day. More than double, because I took one PRN dose daily without fail, to the point the regular nurses didn’t even make me ask for it as they usually do with PRN meds. They knew that along with the meds I was scheduled to take at 9am, I needed a PRN pain pill because that was when I was getting up and ready for the day most days. On my shower days, they usually got to me around 10am and I had to take a PRN pill before going to the shower because sitting in the shower chair was VERY painful. So, coupling the systemic shot with the increase pain meds and all of my other meds, there is NO reason that I was needing to get a shot every few weeks other than the fact that the med in the Medrol shot was just not effective compared to Decadron. That’s just ridiculous to go from needing a shot every few months to every few weeks. So I know that for me, I do react differently to different types of corticosteroids.
Per the Drugs.com Professional page on Dexamethasone (has the FDA Info) “Chemically, dexamethasone sodium phosphate is 9-Fluoro-11ß,17,21-trihydroxy-16α-methylpregna-1, 4-diene-3,20-dione 21-(dihydrogen phosphate) disodium salt and has the following structural formula: C22H28FNa2O8P. Each mL contains dexamethasone sodium phosphate equivalent to dexamethasone phosphate 4 mg or dexamethasone 3.33 mg; benzyl alcohol 10 mg added as preservative; sodium citrate dihydrate 11 mg; sodium sulfite 1 mg as an antioxidant; Water for Injection q.s. Citric acid and/or sodium hydroxide may have been added for pH adjustment (7.0-8.5). Air in the container is displaced by nitrogen.” It’s molecular weight is 516.41.
On the Drugs.com FDA Info on methylprednisolone it states, “Methylprednisolone acetate injectable suspension USP is an anti-inflammatory glucocorticoid for intramuscular, intra-articular, soft tissue or intralesional injection. It is available as single-dose vials in two strengths: 40 mg/mL; 80 mg/mL.
Each mL of these preparations contains:
Methylprednisolone acetate USP ………………………………40 mg ………….80 mg
Polyethylene glycol 3350 …………………………………………29 mg ………….28 mg
Myristyl-gamma-picolinium chloride…………………….0.195 mg ……..0.189 mg
Sodium Chloride was added to adjust tonicity. When necessary, pH was adjusted with sodium hydroxide and/or hydrochloric acid. The pH of the finished product remains within the USP specified range; e.g., 3 to 7. The chemical name for methylprednisolone acetate is pregna-1,4-diene-3,20-dione, 21-(acetyloxy)-11,17-dihydroxy-6-methyl-,(6α,11β).” The structural formula is: C24H32O6 and its molecular weight is 416.51.”
Table 2: Glucocorticoid Equivalencies, Potencies and Half-Life (from an ADVANCE for Nurses Course titled: Corticosteroids: Management of Iatrogenic Cushing’s Syndrome ) shows that prednisone, prednisolone and methylprednisolone are all intermediate-acting corticosteroids. Under long-acting corticosteroids, only dexamethasone is listed. So that may be why I do best with dexamethasone for major flares along with my daily 5mg of prednisone. It’s interesting how many people react well to one drug that is very similar to another that does not help as much. The table shows how much prednisone and prednisolone have in common when it comes to approximate equivalent dose (mg), relative anti- inflammatory potency, relative mineralocorticoid activity, biologic plasma (min.), and half-life biologic (hours). They have the same approx equivalent dose (5mg); the same relative anti- inflammatory potency(4), the same relative mineralocorticoid activity(1), and the same half-life biologic (18-36 hours). Only the biologic plasma is different. For prednisone it is 60min and for prednisolone it is 115-212min.
Used both. They were both effective. With prednisolone I had a lot less side effects.
After my diagnosis at age 7 I was never on anything aside from ibuprofen and naproxen. It was not until I was 25 and had a mega-flare after having my son that I was ever given either prednisone or a DMARD. At that time, the risks of DMARDs outweighed the potential benefits for someone who only had a “mild” case of sero-negative JRA. Sadly, I now pay the price for that lack of treatment in that I have a good bit of erosion, deformities and joint damage. Because my labs have always been fairly good, my doctors have a hard time figuring out whether my RA is active or whether I am just dealing with prior damage. I had one jerk of a podiatrist tell me, without knowing my prior history, that I should be on the high dose of prednisone that I was on (20mg/day at the time) because I had signs of osteoporosis in my feet. I was nice when I explained to him that while I knew pred could cause osteoporosis, especially after using a high dose for an extended time as I had, that in MY case, pred was NOT the cause of my osteoporosis. It likely worsened it but there’s NO WAY it was the cause of it because I had x-ray evidence of osteoporosis a full 13 years before I EVER took a corticosteroid so there’s no possibility the pred caused the osteoporosis, worsened it yeah, that’s a given. But he refused to believe me and I didn’t have my records from nearly 20yrs before with me. That’s not something I carry around. Needless to say, he is a doctor I refused to see again. Neither of my doctors at the time liked that I was on that dose, and neither did I. It caused me to have a scary rapid heart rate (120+), my BP was typically in the 130-140+/100-120+ range. I put on nearly 80lbs over the 2 yrs I was on pred. Yet it only took from Dec 2008-Mar 2009 to get down to under 100lbs due to my constant and uncontrollable nausea/vomiting which is NOT a weight loss program I recommend. The C-Diff helped the weight come off as well. So not a good way to lose weight. Because of the multiple infections and my meds suppressing my immune system a bit too much, I had to go off of ALL RA meds.
But, without pred and Arava, I literally stiffen up so that I cannot move. Sadly, I am not being melodramatic because that happened during those11 mo in the hospital when I was off RA meds and only on IV pain meds, muscle relaxers, Neurontin and the various antibiotics, anti-nausea, shingles, and various meds to heal my stomach. My fingers closed into as tight a fist as they will close, my wrists bent so that my hands were reaching toward the underside of my arm, my elbows bent so that my hands were almost resting on my collar bones. I couldn’t do anything for myself. It took awhile before I could even feed myself again. I had to learn to write all over again, and my then 8 yr old wrote MUCH better than I did and he is a messy writer. It took months before I could feed myself a full meal. I had to have help because I was so slow that food would get too cold to eat before I could eat even half of my meal.
I cannot say whether I do better with prednisone vs prednisolone because as far as I know I’ve not had prednisolone. But I DO know that I react better to some corticosteroids than others. With my previous two RDs, they used Decadron (dexamethasone) for both intra-articular and systemic injections. There was no problem with them doing that with my then insurance company.
When I was at the nursing home, I was in a major flare and asked my dr for a systemic injection. I would loved to have had a couple specific joints injected too but I didn’t think he would do an intra-articular injection and would send me to either an ortho or an RD and at the time, the extreme pain of being transferred would have outweighed the benefit of the joint injection because this was when I was still being transferred by ambulance because my knees didn’t have the range of motion to allow me to sit in the seat of a car. As was normal for that dr, he asked me what I’d had in the past and what worked best for me. He was really great about listening to me when I said what worked and what didn’t. I told him that from 2006 on I’d had nothing but Decadron that I knew of and it worked well, except for the occasional headache afterward, well and the fact it makes me VERY hyper and worsens my chronic insomnia. But that I could tolerate the headache to get the relief the shot gave. And the hyperness was just ignored by those around me. I think my RD gave me 4-8mg depending on the situation. If it was a shot given prior to me doing something that we knew would send me into a flare, like going on vacation, etc. I believe he would give me the 4mg but if it was a flare that had been ongoing, he’d give me 8mg. I know the RD he worked with had given me what she called a “double dose” in the past b/c of the severity of my flare. So my doc at the nursing home wrote the script, the nurses ordered the shot, gave it and I felt better. Then a few weeks later I got a letter from my Medicare Part D insurance co. They don’t cover Decadron, so they had denied the claim. It wasn’t a HUGE deal but it was a hassle. I knew that we could appeal and have the paperwork filled out to show it was needed and get an exception but I did NOT want to have to do that every time I needed a shot, because I knew the nurses were overworked at the time and filling out paperwork for me to get an exception was too time consuming. At that time I was getting them every 2-3 mo because I’d not re-started oral pred daily. So, I asked what they did cover. Their answer was Medrol (methylprednisolone). So I told my doc that was what I needed. I am unsure of the dose he gave me but I can say that I went from needing a systemic shot every 2-3 months to barely feeling any relief which did not last more than a few weeks and at one time only 3 wks passed before I was miserable and begging for another shot. And this is despite having fairly good pain management meds. In fact, he’d upped my pain meds from: 10mg methadone scheduled three times a day with hydrocodone 750 PRN three times a day to 15mg methadone scheduled four times a day and another 5mg PRN three times. It took my total daily dose from 30mg methadone to 60-75mg a day. More than double, because I took one PRN dose daily without fail, to the point the regular nurses didn’t even make me ask for it as they usually do with PRN meds. They knew that along with the meds I was scheduled to take at 9am, I needed a PRN pain pill because that was when I was getting up and ready for the day most days. On my shower days, they usually got to me around 10am and I had to take a PRN pill before going to the shower because sitting in the shower chair was VERY painful. So, coupling the systemic shot with the increase pain meds and all of my other meds, there is NO reason that I was needing to get a shot every few weeks other than the fact that the med in the Medrol shot was just not effective compared to Decadron. That’s just ridiculous to go from needing a shot every few months to every few weeks. So I know that for me, I do react differently to different types of corticosteroids.
Per the Drugs.com Professional page on Dexamethasone (has the FDA Info) “Chemically, dexamethasone sodium phosphate is 9-Fluoro-11ß,17,21-trihydroxy-16α-methylpregna-1, 4-diene-3,20-dione 21-(dihydrogen phosphate) disodium salt and has the following structural formula: C22H28FNa2O8P. Each mL contains dexamethasone sodium phosphate equivalent to dexamethasone phosphate 4 mg or dexamethasone 3.33 mg; benzyl alcohol 10 mg added as preservative; sodium citrate dihydrate 11 mg; sodium sulfite 1 mg as an antioxidant; Water for Injection q.s. Citric acid and/or sodium hydroxide may have been added for pH adjustment (7.0-8.5). Air in the container is displaced by nitrogen.” It’s molecular weight is 516.41.
On the Drugs.com FDA Info on methylprednisolone it states, “Methylprednisolone acetate injectable suspension USP is an anti-inflammatory glucocorticoid for intramuscular, intra-articular, soft tissue or intralesional injection. It is available as single-dose vials in two strengths: 40 mg/mL; 80 mg/mL.
Each mL of these preparations contains:
Methylprednisolone acetate USP ………………………………40 mg ………….80 mg
Polyethylene glycol 3350 …………………………………………29 mg ………….28 mg
Myristyl-gamma-picolinium chloride…………………….0.195 mg ……..0.189 mg
Sodium Chloride was added to adjust tonicity. When necessary, pH was adjusted with sodium hydroxide and/or hydrochloric acid. The pH of the finished product remains within the USP specified range; e.g., 3 to 7. The chemical name for methylprednisolone acetate is pregna-1,4-diene-3,20-dione, 21-(acetyloxy)-11,17-dihydroxy-6-methyl-,(6α,11β).” The structural formula is: C24H32O6 and its molecular weight is 416.51.”
Table 2: Glucocorticoid Equivalencies, Potencies and Half-Life (from an ADVANCE for Nurses Course titled: Corticosteroids: Management of Iatrogenic Cushing’s Syndrome ) shows that prednisone, prednisolone and methylprednisolone are all intermediate-acting corticosteroids. Under long-acting corticosteroids, only dexamethasone is listed. So that may be why I do best with dexamethasone for major flares along with my daily 5mg of prednisone. It’s interesting how many people react well to one drug that is very similar to another that does not help as much. The table shows how much prednisone and prednisolone have in common when it comes to approximate equivalent dose (mg), relative anti- inflammatory potency, relative mineralocorticoid activity, biologic plasma (min.), and half-life biologic (hours). They have the same approx equivalent dose (5mg); the same relative anti- inflammatory potency(4), the same relative mineralocorticoid activity(1), and the same half-life biologic (18-36 hours). Only the biologic plasma is different. For prednisone it is 60min and for prednisolone it is 115-212min.
I have another wrinkle to add to the question. My GP had me on low doses of hydrocortisone/Adreset (another sister to prednisone) twice daily to help with low energy level related to what she thought was adrenal fatigue. It was when she tapered me off of the hydrocortisone (after taking it for 2-3 yrs) that -BAM- swelling/pain appeared and I was dx’d with RA. Seems that little bit of this med had held the RA at bay. I’ve ended up on Sulfasalazine & Plaquenil which are controlling things for now.
When I have taken Prednisolone I gain a lot of weight is this normal It does help but can’t stand the many extra pounds!
Deb Wilden
Deb, not everyone gains weight from prednisone, but I think a majority do. It is a common side effect. Maybe you could ask your doctor about lowering your dose or helping you find a solution such as maybe swimming or something that burns a lot of calories, if you’re able to do it. It must be frustrating.
kelly
Thanks for your reply I will ask to take a low dose. I was doing a swim exercise class, but stopped because of extreme back pain which I found out was from the ra as well. So you are giving me hope that something could help, so I could get physical again. I kind of just stopped everything once diagnosed with ra I have been so depressed, felt like I couldn’t hardly move. Plus the medications have made feel very off balance and sluggish. They just lowered my dose of sulfur to see if that will help me feel better.
Deb
I know how you feel and you can only do what you can. No two of us seem to be exactly alike. And, the disease can also change over time in the same person. So never give up hope. There’s also the hope you’ll get to a point with the right combination of meds & your body adjusting to them so you can do more than you can now. Just don’t beat yourself up either way.
I was on Prednisone for 9 years. The last 5 of them was an extremely low dose (5mg/day). I decided to try to come off of it and with my MD’s help began a slow taper that stretched over 2.5 months. A few weeks after my taper was complete I had an appointment for some routine lab work where they discovered that my blood glucose levels were below 40! AND this was after breakfast of sugary cerEal! I was sent to an endocrinologist who monitored my food intake and blood glucose for a month and also ran several test on me. He finally came to the conclusion that my adrenal glands had shut off bc of the long term Prednisone use and that they were not producing ACH (?) that helped to regulate my blood glucose levels. I was diagnosed with Reactive Hypoglycemia, but they hope that it is temporary. My MD thinks that once my adrenal glands “wake up” and start functioning on their own that the Reaction Hypoglycemia will resolve itself. I was put back on a steriod (Hydrocortisone this time- a little easier on the body) and am a year into the treatment to try to stimulate my adrenal glands with no luck yet. I now not only struggle with RA but Reactive Hypoglycemia as well. Which means that about an hour or two after I eat anything my blood glucose bottoms out.FYI: Fatigue+Low BG= No fun! If I could hop in a time machine and go back 9 years ago I WOULD HAVE NEVER TAKEN PREDNISONE!
I got very good results with 10mg of prednisone but Doc cut me back to 7.5mg and I can tell the difference. His goal is to take me off the prenisone all together. I don’t recall any side effects.
Kelly, you are a godsend for recognizing the differences and taking the time to post them here. I am one that has no relief whatsoever from plain prednisone. Medrol (Methylprednisolone) is a whole other story, though. If you hadn’t posted this, I might not have realized that connection. I was always given the Medrol dosepak for acute infections and I felt like Superwoman (even with a sinus infection)! However, my doc put me on Pred for 7 mos. and I gained 70 lbs and had no relief! I’ve now been on 8mg/day of Methylprednisolone and my joints are so happy and I’ve LOST 50 lbs because I can actually move again! I am so grateful that my uber-genius new Rheumie agreed that there certainly is a difference in the metabolic process. God bless you, Kelly, for your dedication to help others. I wish recovery for you every single day. If we both felt good (at the same time), it would be my pleasure to advocate for you on behalf of all autoimmune patients! Much love and sincerest appreciation.
~Lynn
Lynn,
I am so glad you mentioned Medrol (methylprednisolone)! I have hated using prednisone or prednisolone and would always refuse them due to horrible side effects. I never can sleep and have terrible dreams. Mind and body just race.
However, ever since I was a teenager, my old school primary doc would give me Medrol injections to calm sever allergy attacks with minimal side effects for me. When my Rhumy heard that she immediately suggested we try 4 mg Medrol tablets. I can take one a day if I wanted, but all I need is a half tablet (2mg) every other day along with my methotrexate injections and low dose Imuron.
I have terrible side effects to many drugs. I have been through 4 biologics in 3 years. I wanted them to work, but they never did long. What it seems to help the most so far is a cocktail of low doses DMARDS. Imuron 25 mg. twice a day. MTX preservative free injection 7.5 mg once a week (with 3 mg folic acid per day) and now 2 mg Medrol every other morning. Plaquenel however made me contemplate suicide, just out of the blue one day, after about 6 weeks on it, so that one is a no go.
I am far from pain free, but at least I am walking again and my brain is working again. I finally feel like I might be on the right track.
Prednisone was my like my miracle drug. I was put on 25 mg per day when I was first diagnosed. Within 4 hours of taking my first dose I was 50% painfree! It took a few weeks for the full affect to happen but it was incredible. I don’t recall any side effects that bothered me too much. I was weaned off after about 3 months and I’m now on a cocktail of methotrexate, plaquenil and arava with just some minor pain off and on.
Prednisone for me…is also a wonder drug! I become the ” old me “…the one with loads of energy, no swelling ( I can wear jewelry again ) and minimal pain. At higher doses, 10mg., the sleeplessness occurs, but, I have taken Ambien for that.
Currently, I am taking 4mg. a day of methylprednisolone. Have been on it for 3 months now, and it’s losing it’s effectiveness. I see my Rheumy in 2 weeks and I know it’ll be time to wean off. Not too excited about that, since I know the masked symptoms will all return.
My rheumy used a taper week of prednisolone to help with RA diagnosis a year ago at age 53 and it helped the pain immensely.
While on Methotrexate/Plaquenil we used monthly injections of prednisolone for 3 months. I forget the dosage… It was a great help and bridge. Each injection lasted about a month with NO side effects. But the Meth made me so sick, I switched to Arava in January with one week of prednisolone taper to bridge until Arava kicked in – which it has! I’m doing very well on Arava/Plaquenil and the occasional Aleve.
Then my Plantar Fasciitis got worse this past spring and doc gave me another week of Prednisolone taper. It worked really well and no side effects.
I have been on and off prednisone for almost 4 years. this latest round has been a very slow withdrawal as I await the certainty of the effectiveness of my orencia infusions. now I am at 2 mg daily and starting to get flare ups again – also I am losing the excess weight the higher dosages caused for me and I feel all around calmer perhaps a bit “depressed”. I am determined to get off the prednisone so I will wean these last 2 mg down a half mg at a time over the next 3-4 months. I don’t really careabout weight gain compered to the severe pain of flare ups – esp in knees and shoulders – yikes! I will ask about the prednisolone at my next office visit.
Prednisone 10mg works for me. I’ve been on for about 4to5years.Also been on Humira,Rituxan,and Enbrel they didn’t work so well,now I take Xeljanz 5mg and for the first time in months my feet are going down and I have very little pain,Been on Xeljanz 1 month.
I’ve been on low-dose prednisone for almost 30 years. Never more than 10 mg, but I still have some bone density issues because of it. It does make it harder to lose weight, too. I adjust the dosage myself when I have a flare and, thankfully, have a good rheumy who knows that I’m not an idiot who will be endangering my health. He trusts me to know what I’m doing and to know my own body. I’m fairly sensitive to prednisone and can only taper in 1/2 mg increments and that’s what I use when increasing it, as well.
I’ve never tried prednisolone, but prednisone for me has been great, aside from the lower bone density. I wouldn’t be able to move without it. I just wish my bones didn’t have to pay for it.
My Rheumy prescribed Prednisone 60mg. The very little benefit I had was not worth the horrible side effects. So my rheumy weaned me off. Then about a year later I was hospitalized and they couldn’t find anything to get my pain under control. So my Rheumy ordered I be given a high dose of Solumedrol via my IV (basically given Prednisone via an IV). Before the nurse had even left my room after starting to give me SoluMedrol via my IV I started having an Asthma Attack. So the nurse stopped the prednisone and called Respiratory therapist to give me Albuterol breathing treatment. Obviously I didn’t not receive any more Solumedrol. The next day my Rheumy decided to try Prednisone in a Pill form since I had been able to take it before. 15 minutes after taking the pill I started having difficulty breathing again. 20 minutes after taking the pill I was in a full blown Asthma attack. Again I had to have Albuterol breathing treatment. After the second attack I was informed by both my Primary Care Physician and my Rheumy to always list Prednisone on my medication Allergy list. I was also told by both of them that if I ever have to see a doctor I have never seen before they probably will not believe that I am allergic or that, my allergic reaction is an asthma attack as prednisone is often used to treat asthma.
Andrea, it may be rare to be allergic to prednisone, but you’re not the only one. I know someone with the same reaction to prednisone, and he has commented about it. If I can find the link to his comment, I’ll paste it here for you.
Did you say that 60mg per day gave you very little benefit? Or was that a shot?
I have now been only on Pregnenolone 25 mi from a natural Dr. Also a slew of Vitamins my pain has gone from a 10 to a 2 and almost gone.
Deb
FYI for those who aren’t aware of it, if you get bronchitis or a bad chest cold, make sure the doctor knows you’re on steroids. I’ve been told by multiple doctors that the corticosteroids like prednisone can mask the symptoms, so they won’t necessarily hear the congestion when listening to your lungs. They told me that it means I can risk getting pneumonia if it’s not correctly treated.
Isn’t taking meds so much fun? 🙂
Hi
I was just reading about responses to Prednisolone and Prednisone.
I was very confused by this as I heard that they are miracle drugs for ra. I am seronegative and still looking for the right combination for me.
I had a double dose of prednisolone injected systemically in each shoulder with no response. I have also been on a prednisone
also with no response.
Just goes to show how heterogeneous the disease is.
so II have aero negative ra that has been progressive. The first time it had pred I needed 20 mg a day and it worked great, but the we tapered and precipitated full body flare. I was then on 30 a day still with full body joint pain, not sleeping and ended up in the ER with stomach ulcers and esophageal spasm even though I was taking ppi’s. I switched to long acting pred injections at high doses and they have only worked for 3 weeks rather that 6 to 8. The whole thing has been super frustrating. I saw another rheumatologist and he said that he thinks I’m a nonacytalater, so can’t activate pred, the same as the t3 example. We’re trying me on dexamethasone now while we’re waiting to see if adding sulphasalazine to the methotrexate will kick this. I’m still taking 80 mg of proton ix a day so I’m a bit nervous but he says dex typically works for nonacytalators, so we’ll see… I’m think I’m headed to a biologic, but am a little iffy as I work with kids and I know someone who developed lymphoma from them…..this is all such a pain! ( literally too!)
For those who react negatively to Prednisone, I thought I would share my experience. I too cannot take Prednisone for all the reasons others have mentioned. Unfortunately, aside from Remicade, I have tried every drug on the market for my RA and I have had horrible side effects to them all except sulfasalazine and steroid. I take the sulfasalazine because I can but I don’t think it helps. However, I have been on Medrol (methylprednisolone) for 20+ years, 4 mg per day (not dose pack) and it has been a life-saver for me. My bone density is fine. No changes after 20+ years and I am 53 and post-menopausal. My eyes are fine. I bruise very easily but that is not problematic. My RA has not progressed for years (confirmed via MRI). The serious side effect is that my body produces NO cortisol on its own now and my adrenals are bottomed out. I cannot go off the Medrol. That is clearly not a positive, but if I had been on a biologic etc. I could have cancer, TB, or any number of diseases….or be dead. Every drug option we have is awful and toxic. For 20 years of daily steroid use, I would choose to take and stay on the Medrol again. I’m grateful that although I can’t go near Prednisone, Medrol works for me. That may be an option for others to explore (but I don’t think most docs prescribe Medrol for daily use). My body loves it though!
I get slow results.at 10mg the vest are at 25mg. Fortunately I am off them completely. At least for now.