Rheumatoid Arthritis Swelling, Take Two
Rheumatoid Arthritis Swelling (UPDATED 2016)
In honor of the blog’s 2nd birthday, let’s consider some issues that have been significant over the last two years. Today we’ll consider Rheumatoid Arthritis swelling. This may be blunt. More like a frying pan than a sword.
Talking turkey on Rheumatoid Arthritis swelling
A couple of years ago my kind-but-clueless-what-to-do-next (her word) rheumatologist told me two things that provoked my online journey to go deeper and farther. After two and a half years on high doses of Humira and methotrexate, my RA symptoms were not improved. Disability progressed even though obvious external swelling had mostly subsided.
Two significant things Dr. KBC (kind-but-clueless – her word) said:
1) I don’t have a clue what to do with your RA. It does not look typical any more.
2) You cannot have x-rays done because you have a systemic disease. There’s no justification for x-rays.
I searched online for patients like me. I searched for some kind of explanation why my RA hurt more than ever, with constant fevers, and joint instability. Why did some claim those symptoms are only possible or relevant if obvious external swelling is present?
I listened to patients and blogged for almost a year before I made my Rheumatoid Arthritis swelling confession. But, there are 224 331 358 370 replies on that post. If you’re confused about Rheumatoid Arthritis swelling, you could learn a lot there.
When I got the courage to leave Dr. KBC, I met a series of rheumatologists who either insisted that I was in remission or that I really have fibromyalgia because my “inflammatory indicator” CRP and my swelling both say I’m fine. Each of them was adamant.
Like Goldilocks, I held out for the one that seemed just right. Did you see me cry in the Good doctors treat patients video? We were overjoyed to finally meet Dr. Smart Rheum who said wonderful things like this:
- “You DO have swelling. I can feel it when I examine your joints.” (Examining my joints was a novel experience.)
- “Tests don’t always show disease activity. You have to look at the patient. It’s the patient that matters.”
- “What do they mean ‘You don’t look like you have RA? What does RA look like?’”
- “Swelling does not have to be on the top of your hands. The other side is swollen.” (Where the tendons are.)
Last week Dr. Perv told me “You have no kind of arthritis at all. You have no swelling. You claim to have pictures of swelling, but you have none.” I said, “My knees are swollen right now-” “NO they are not!” he interrupted without ever looking at my knees.
Note well: most “asymptomatic” patients have synovitis & bone edema
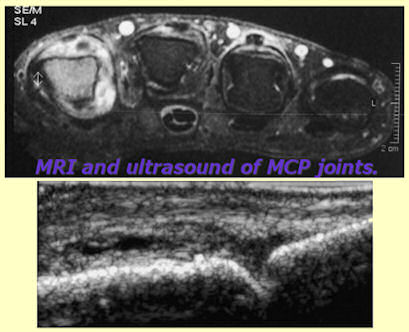
There are some links to support our case on that first swelling post, but there’s one I somehow missed until recently. Dr. Brown’s study at the American College of Rheumatology (ACR) in 2006 showed that patients who rheumatologists label as “in clinical remission” due to lack of visible symptoms are experiencing damaging disease activity. Active synovitis and internal swelling can be detected with skillful use of the appropriate tools. Bone marrow edema is another critical unseen aspect that doesn’t look like RA to the naked eye.
“Even in asymptomatic patients with clinically normal joints, MRI showed that 96% had synovitis and 46% had bone marrow edema, and ultrasound imaging showed that 73% had gray-scale synovial hypertrophy and 43% had increased power Doppler signal,” they report. Mild synovial thickening was seen in three of the 17 control subjects (18%), but none had bone marrow edema. Brown et al point out that synovitis in RA is a link between inflammation and structural damage and they predict that the patients in this cohort who had synovitis are at risk for subsequent structural damage. They suggest that such persistent, active synovial inflammation may explain the adverse RA outcomes seen even in patients who meet the ACR and DAS28 criteria for complete remission. This is a large study and needs to be taken seriously,’ said Professor John R. Kirwan, consultant rheumatologist and professor of rheumatic diseases at the Bristol Royal Infirmary, in the UK,” RA Remission Often Accompanied by Silent Synovitis.
Was it? Taken seriously? Maybe more rheumatologists need to hear about it.
Now I finally have persistent swelling. My knees have had Baker’s cysts behind them for almost a year. They’ve been painful and stiff for five years, but now I have something that brings a little sympathy. The fronts of the knees also swell periodically.
“Asymptomatic” is in the eye of the beholder.
Now I have an opposite problem. They deny that THIS is swollen.
Read my lips. I’m. Thin. These are not fat knees. They are swollen.
I went through the same thing with my pregnancy with Roo. My feet were can’t-wear-shoes-huge, but the midwife said they weren’t swollen. After Roo was born she remarked, “Oh my god you’re right – your feet are skinny.”
Enough.
We don’t have time for it. We are supposed to be treated “early and aggressively.”
How can we be if so many doctors don’t recognize RA because they have a wrong mental picture of it?
So why does this myth persist?
Happily, others are speaking up about Rheumatoid Arthritis swelling also.
Edit: Link to original Musculoskeletal Report article updated to a current link to the Brown swelling study, here:
ARTHRITIS & RHEUMATISM
Vol. 54, No. 12, December 2006, pp 3761–3773
DOI 10.1002/art.22190





This post got my blood pressure worked up! All I can say is find a doctor that will listen to you. Yes, I truly do understand how difficult that can be but please, please, please keep looking. If we could treat ourselves with these terrible diseases that would be different but we can not. I also had the “no swelling” issues but I have terrible joint damage now. And like you I took all the high potent meds with no relief and no improvement in my joints. What has frustrated me the most is I did the ra dance with these docs and danced to their steps to only wind up with terrible joint damage. And I can’t tell you how many times my crp was low and my joints weren’t that swollen but I was in terrible pain and felt terrible. Just know you are not alone in this and that your symptoms are real and that your pain, fatigue, etc. is real. Your job is to find a doctor that will listen to you. And listen carefully to all that is going on inside of your body. I HATE that these docs use these measures that are so false. I am beginning to think they use these measures because if they used patient measures…all these drugs would fail miserably.
I think your suspicion might be right. Creating a rosy picture seems to be the goal of some involved in rheumatology instead of creating an accurate picture so that there can be accurate research. No one is glossing over lupus or diabetes or cancer – they research the real disease.
You know, I feel for you. I understand and feel EVERYTHING you have gone through. I am glad all these doctors have gone to school, become educated in their field, but just because they have a degree doesn’t mean they know everything. I have a feeling in their education, they only see “typical” cases and their texts don’t have anything like what the _real_ people experience.
My first rheum, when I said my ribs hurt, a lot, when I breathe, that my back is in pain, my neck, and that my hands are rarely affected (that was nearly 3 yrs ago) she said it was only fibro and the ribs hurt because of muscle spasms.
My current rheum redid all my blood work and actually examined me. Took xrays. My blood work proved my inflamation and pain. However, that was last July. I’m beginning to get frustrated again, because the relief I felt before is gone. I am wondering if it wasn’t just all in my head, wanting things to work, because someone listened and was treating me. Or, have I outgrown the treatment?
My knees, hips, back and shoulders swell a lot. My hands only periodically. My toes and ankles swell a lot too. But, true to most of my “luck” – the swelling goes down when it’s time for my appointment. It’s frustrating. And, I’ve noticed that the only part she checks is my hands. She will check other “pressure” points on my back and elbow, ankles.
We need to find a way to rewrite their books. So they see that nothing is TYPICAL about our disease.
Bad luck if one’s hands swell the least with a rheum doc who is most interested in hands. That would be another on my top top myth list – that RA should be measured by what it’s done to the hands.
Right on que! And how many docs miss what ra has done to the heart, rib cage, ligaments, veins, jaw, neck, etc. etc. This disease can be deadly but unfortunately alot of docs are just holding our hands in this dance. Pun intended.
Good one. 😉
I think that even if you came into that mans office looking like the elephant man he would have still denied your obvious swelling sweetheart and obviously is not a good doctor and should not be practicing.
I am very small framed also and have had very similar comments as you before. I also have bakers cysts at the back of my knees. I wonder at times now how my joints are supposed to look because I have been away from the norm for so long.
I hope you find a new Rheum that will listen to you and properly assess you.
As always, thank you for what you do… Finding your blog in my inbox every morning is as mandatory as my cup of coffee 🙂
Aimee xoxox
Weird how being thin works against us w/this disease. Swelling is less dramatic looking and our crp is lower since higher bmi yeilds higher crp. Weird especially since weight loss and low bmi are “classic” symptoms of aggressive RA.
You know, it is funny because I am thin too but I can so see and feel the swelling but my dr. can’t. My cpr levels are good too. I didn’t even think about the correlations between CPR and BMI because my BMI is low since I lost sooo much weight when I got walloped by RA. I even will show my husband how swelled they are and he says they just look really thin to him. I guess that is true but then why can’t I get my rings on? UGGGG!
exactly. my rings got smaller and smaller. when the skin was swollen over the wedding ring bad enough, I had it cut off 1 1/2 yrs ago. The mark is still there on my finger where the ring was squeezing it. My fingers are just much larger. Not puffy. But bigger. Lots of RA patients tell me that – and it’s not weight gain.
Yep, that’s me, too. I used to have skinny, petite fingers. Now, besides the ugly nodules, my fingers don’t look unusual to most people…but they sure do to me! It comes and goes to some degree, but I have a feeling some of it will never get back to “normal”. Fortunately, I had a couple rings that I never got sized (they were at least a couple sizes too big) – now, on a good day, I can at least wear those ones 🙂 My wedding ring is stuck on; I’m just hoping the swelling stays around my middle joint so I don’t have to cut it off!
It is so funny because my RA dr. says there isn’t swelling in my hands anymore but yet I can’t put my rings on and I am 25 pounds lighter than before RA. and I was thi
then. Obviouly I lost no weight in my knuckles and they mysteriously got bigger! Hmm, doesn’t make sense to me! My husband ended out cutting my wedding ring off with a pliars. I would not recommend this method!
I’m sorry if I confused you. This post is not about me.
In choosing some of the top issues from the last 2 yrs that still need to be addressed, swelling is one of the biggest.
Too many rheumatologists are confused on an issue that has been settled by science. There can be and is active RA with negligible external visible swelling in a majority of patients.
I wasnt confused at all Kelly. I will, however, disagree with you. This post is about you. You are a RA Warror and this post is about every RA Warrior out there fighting. I sat here reading this post doing the happy dance. I love it when I come on here and find my thoughts presented in such a coherent manner. (must adjust my tin foil hat your reading my mind again lol) My very first (and favorite) rheumy was a NP that had RA herself. She did her exam (very completely) and noted synovitis everywhere. When her MD came in his exam was quick, rough and very painful. He said it was all tendonitis, bursitis, and I my joints were fine. After he looked at my blood tests he came back and examined again (quick and rough) and changed his mind there was some synovitis. As my swelling receeds, I am fasinated by my different body parts, I have forgotten what normal is suppose to look like now. This isnt “anti doctor” because every other MD has had no trouble finding my synovitis. It is about the differences in the education, evaluation and reality of RA.
tin foil hat! so you admit the post is about you too. lol. that’s what I meant. I don’t want anyone to miss the forest for the trees. Whether I have a rheumatologist yet or my knees get treated is not as big an issue as fixing this big problem that so many doctors think that if they don’t see dramatic swelling, they don’t see RA.
Oh, thank you so much! My previous rheumy told me I wasn’t swollen at all, and since my ESR and CRP were “normal”, I must have fibromyalgia! Yeah, and he didn’t even touch my joints, either! I went back to my old rheumy, even though he’s an hour more drive. But, I got a REAL doctor again! Thank you so much for posting this!!!!!
Being new to all of this, diagnosed in February of this year, I’m still trying to understand everything about this disease. Your website has been a blessing. My rheumatologist was eager for me to have a new RA test recently. It’s called the Vectra DA test. It tests 12 biomarkers, including CRP, to determine disease activity. I don’t know if anyone has heard about this test, but maybe it would give a clearer biological picture for those patients who are “asymptomatic.” I myself seem to be in the “typical patient” category with symptoms in my hands along with the swelling, but I have compassion for those of you who suffer greatly with the pain and the skepticism from others including your doctors.
Kelly, can you get your primary care doc to take x-rays, at least of your knees? I can’t believe that response from Kind but Clueless rheumy that there was no reason to take xrays because “you have a systemic” disease! Why would he/she put you on methotrexate and biologics WITHOUT EVER TAKING XRAYS?????
My rheumy was not a big one on doing lots of tests and xrays (except for CBC and CMP to monitor methotrexate). But did do xrays if I requested. But I have some obvious damage and these parts were xray’d(in addition to non-obvious RA changes but those weren’t xray’d). I didn’t ever get into discussions with rheumy about why not doing xrays of other typically involved parts. ie – cost, radiation exposure, or doesn’t feel need to xray unless EXTREMELY bothersome.
You need to find a primary or rheumy willing to xray those parts bothering you. Hands, knees, feet, shoulders and neck. I would think that previous rheumy would have had to have some of those to justify to the insurance company to get you on biologics in the first place.
The research on non-visible swelling and bone marrow edema is intersting isn’t it?
She never took xrays. I had a high ant-ccp and an elevated Rf. I had severe swelling in my toes. I don’t think “no xrays” is unusual, from what other patients say. This is actually the part 2 that I was hoping to write today or tomorrow – about this question of testing/imaging standards.
I have a theory that I describe pain in too many joints in an appt. Dozens of joints hurt daily. At least 10 of them over an 8 each day if I let pain meds lapse. I can’t put weight on one knee or hip or ankle many days. My shoulders and neck scare me… if a patient says all that, a doctor shakes his head. I’m thinking a more effect strategy would be ONLY complaining about my knees until they are treated, etc. That’s how I finally got finger injections last year – making an appointment to only talk about that.
On the research, there’s no excuse that the average rheum doc has no idea about this and patients are here discussing it. It’s 4 or 5 yrs old.
Kelly,
If I’ve asked you this before, my apologies. Have you had your vitamin D serum levels checked? Get the 25(OH)D test. Your PCP can order it. (in fact it was my PCP who caught my deficiency).
Both my rheumatologist and neurologist advocate for a serum level between 50-80 ng/mL for their autoimmune patients. Much of my overall pain was relieved as my levels rose from an extreme deficiency of 7.8 ng/mL.
Lisa
Yep, I think you’re right. Pick the one area that has been bothering you the most and make that your main focus of the visit. Rheum docs are under time/insurance constraints just like primary docs.
I was not thinking of time contraints. I was thinking of crediblility. It seems to be just too hard to belive that a person has active RA in all joints at once.
I have to admit that whle I’m intrigued w/this idea, my kids were mortified at the thought that I’d wait 3-6 months between treating joints. That could be 30 years before we got to look at all of the ones that hurt. I laughed – at least that’s a start. Right now, it’s been 5 yrs and I’ve had 2 injected – an even slower rate.
Wow, what a timely post for me. My appointment with my rheumatologist this morning ended with me sobbing while she stomped out of the room. She just kept telling me that since she can’t see any swelling she can’t treat me with anything more than plaquenil. She refused to believe that my swelling is very subtle because she’s never seen it. She got very angry when I said that I didn’t think that it was fair that she was basing that on the three very appointments I’ve had with.
Needless to say, I won’t be going back to her. Unfortunately, though, that leaves me with just one more option for a rheumatologist. I see him in June and if things don’t go well, I’m not sure what to do. Today’s appointment has me seriously thinking about trying to get back in with my first rheumatologist back in Portland. It would be financially difficult to fly back for appointments, but I’m starting to feel like that is really my best option.
-Erica
Erica, thanks very much for telling your story for others to know they aren’t alone. I get enough letters like this and have seen it first hand so that it truly puzzles me. I’ve spent the couple of years trying to figure out why they get so indignant about this. What is so upsetting about a patient telling their symptoms and asking about treatment options? I’ve had them be sarcastic or shout at me that I must admit I don’t have RA because of little swelling or low CRP. My demeanor has always been submissive, never challenging them. I never quote a statistic or act like I know anything. Yet just claiming that it hurts without dramatic swelling infuriates them. Why? Why don’t they know better? And why does it make them so angry?
PS: I’m sorry you experienced that.
Erica, is that Portland, OR? If so which Dr.? I live near there and info would be appreciated. Having trouble finding a doc!
Yes, it’s Portland, OR. Her name is Dr. Mollie Thompson at NW Rheumatology. Really great doctor and a really great rheumatology group.
🙂 I could stop seeing my doc and just read your blog–if I didn’t need MTX and Remicade. You nailed it. He tells me that my RA is in remission due to lack of swelling. He tells me it’s Fibro that is causing my pain. And yet… sore feet, random screaming fingers, hands so weak, they can’t hold on to a thing…and middle fingers that are curled around imaginary triggers when I awake. Fibro?? So, what to do? Start looking for a new doc?
Linda, If you start looking for a better doctor, maybe it would be a good idea to keep that to yourself until you find her/him. You should be able to bring in some lab results or xrays to consult a new doctor without even telling the current doctor about it. Fibromyalgia seems to be some kind of scapegoat for patients who don’t get much better with treatment. Painful joints in RA patients is likely due to RA. It would be good to have some of these imaging tests on our screaming joints, wouldn’t it?
Yes, it would be good to have images of our screaming joints. Need them to either prove you have RA otherwise, or to prove that they are worse and current treatment is not helping. If it’s not going to make the doc change treatment then I guess they aren’t worth having is what the docs think. You can, as you have found Kelly, have two extremely different opinions by radiologists, depending on whether they are very familiar with all the changes that RA can cause. The readings between two sets of hand xrays of mine, although there is obvious extensive damage in both from years apart, read like night and day. You can tell the first radiologist really cared about their work and the second one didn’t appear to give a cr_p at all. I should send you the descriptions. You’d be shocked. I could’ve used the first radiologist to read the second ones as I was considering surgery and that would’ve been helpfull in determining some things.
I just think images are helpful to know how to treat. Usually there is SOMEthing that can be done and the questions are what? and when? Without the images, nothing is done. So many tell me, “I got the mri & then we decided ____.”
Just came across the term “muscoskeletal radiologist” the other day in doing some follow up reading on these discussions/articles. That’s what we need – our imaging tests read by sub-specializing radiologists.
How many of you in pain/fatigue but without obvious swelling are on prednisone when your doc thinks you are in remission or don’t have RA?
There must still be some controversy amongst docs as to whether prednisone just deals with symptoms or whether it has some damage reducing or damage slowing capability. I’ve been on it pretty much continuously since a few months after my diagnosis. It certainly helps dampen down symptoms for me, and yes, perhaps slowed but not necessarily stopped damage. However, it’s time to come off to avoid other side effects and to try to get ready for surgeries (it can hinder healing).
Before I moved I had a rheumatologist who would shake his head, laugh, and put up his hands while saying “the immune system is a funny thing”. That meant I didn’t match the book AGAIN but he believed me. He also did testing which verified that without joint swelling the disease was still doing vascular damage and that rheumatoid cachexia (muscle wasting) was occurring. I think true “remission” is a myth. Some of us just go through cycles of greater and lesser swelling.
What did he use to test cachexia? True remission is very rare, yes.
My primary care doc had detected high protein levels and low fasting blood sugar during a routine annual physical. He shared the results with my rheumatologist (since the comprehensive metabolic panel screens for liver issues associated w/ methotrexate he shared the results to save duplicated labs). In any case these results led the rheumatologist to conduct a bioimpedance analysis which is a painless 5 minute in office test that uses an electrical current to analyze body composition including fat to muscle ratio. The ratio showed an abnormal amount of fat for my height/weight ratio and lifestyle working and chasing young children. The combination of factors led him to conclude that the fatigue and pain without swelling were related to RA related muscle wasting.
Thanks for the information. Sounds logical. I’ll look for more information on using that test for that reason.
I am fortuante to have been referred by my PCP to a great rheumy right away. I had knee issues even in my teens and finally ended at an orthopedist who did arthroplasty many times over the years. When I was unable to walk anymore (@ 43, 8 yrs post diagnosis), my orthpedist could “see” the joints w/ MRI and discovered my L Hip had collapsed. After bilateral hip and knee replacements, he continued to deny my RA, telling me that my damage was from OA. All joints were affected with necrotic bone. When I finally had to have my first shoulder “cleaned out,” the orthopeist, whom I really like, showed me pictures from the surgery and apologized. He told me that all the prior surgeries (about 15) of the lower extremities had not looked “typically” RA but that in my shoulder he had finally seen the “typical” RA joint. My rheumy called it a textbook pic of active RA. This ortho doc is nationally known and has a philosophy that has enabled me to remain as active as possible. He is in his early 60’s and widely recognized for his progressive treatment. I am blessed to have these two docs in my life…the rheumy who has always said I have RA and the ortho that always denied it until a yr ago, 24 yrs post diagnosis. So…is there ONLY one RA? Is RA an umbrella? You are the most aggressive lay person I have ever read. Please continue your search and know you are not alone. I appreciate your efforts beyond measure. Thank you.
Just one more comment about hands…in order for me to assess their degree of swelling, I bought several cheap but sized rings. The rings are a completely objective assessment since the circumference is constant. It is not your imagination…your hands are getting bigger. I am a very large framed woman who wore a size 7.5 ring on my thin prediagnosis whallop. Over the last 25 years, my fingers are now about a 9 but it takes a 10 to make it over my middle joint. Maybe this idea will help others. Prayers to all my fellow warriors.
Wow. this is how I finally knew I wasn’t crazy or imagining things – my rings. Just 2 years ago I wore a new custom-made wedding band ( made just 2 years ago), another band with it, and a ring on each thumb. Now, the 2 wedding bands can’t get on my finger past the middle joint, despite my weight going from 120 to 110,the left thumb ring now fits on my wedding finger, and the right thumb ring now fits my left thumb. Nothing fits my right thumb. I have tiny hands, and now my doc doesn’t even need x-rays – you can see the widening and damage. And I’m sero-negative – ANA positive. And this happened in less than 2 years.
yvonne
That’s a great idea! I also usually have little visible swelling of my fingers, though my old GP could see it (even when I couldn’t!) and he is the one that diagnosed me with RA. My new GP (thanks to insurance… or lack thereof… issues), while he has started me on MTX (and I brought him pictures of my hands when they were obviously swollen during a bad flare) insists on putting down the diagnosis of arthropathy (which I suspect has something do do with why medicaid denied me).
Anyway – I love your ring suggestion, and have another, perhaps cheaper one to offer – I make jewelry and have a cheap plastic ring sizer (it looks like a board with holes in it -made to size fingers, as opposed to the rod type deal that measures rings). I think I paid under $5, so that might be a cheaper option than buying several rings… just don’t get your fingers stuck! And I’m going to start using it and taking pictures so he can see that there is swelling even if it’s not that visible (especially on doctor visit days…). Thanks!
Years ago, when I had a rheumy who was less than sympathetic about my not being able to exercise as I was in a constant state of flares, and would not give me any pain meds at all, I changed docs. There were only 3 rheumys there, including this crappy rheumy, and one wasn’t taking new patients at all. I called the 3rd one, explained that I wanted to treat my RA more agressively (I was 25) and the doctor even called me to discuss it and then scheduled me in. He was great! And I ended up having two total knee replacements less than a year later. Turns out my knees were so contracted, the docs were amazed I was even able to stand at all (albeit bent).
Point is, do NOT be afraid to change rheumatologists! All you really have to say to a new rheumy is that you are not satisfied with your care, that despite treatment you are still having symptoms (pain *is* a symptom!) and if they are any good at all, they will understand. Or you could call it a second opinion if that makes you feel more comfortable.
One of the best rheumys I ever had told me that x-rays and other imaging techniques do not tell the whole story. He said some folks seem to have little pain, and yet have terrible x-rays to the extent that it is a wonder they are even walking. Other people can have the opposite, where their pain is immense but doesn’t show on x-rays or MRIs. We never discussed lab tests and/or inflammation in specific joints, but he seemed to really understand that patients are individuals who do not all exhibit the same symptoms.
Please, if you are not satisfied with the care you are receiving, do try to change doctors! And if you have to go a long distance to find a good rheumy, know that they can often work well with your local primary care doctor in a consultative role as well.
I hope this helps some of you out there! We’re still trying to get my RA under control, but it isn’t because my rheumy isn’t good. It’s just a frustrating, too-often too-difficult to treat disease.
Mary, THANK YOU! for helpful, awesome comments. “Pain is a symptom.” And we must keep trying to find a good doctor so we can get good care. I think I’ll read this one again tomorrow for encouragement.
Just wanted to thank you, Mary, for that comment. I really needed to read that today.
Portion of a later article by Smolen citing back to the main article cited here:
Rheumatoid arthritis joint progression in sustained remission is determined by disease activity levels preceding the period of radiographic assessment
“…Although there was a virtual arrest of progression of radiographic scores at the group level in patients who maintained remission between month 12 and month 24, some patients in all 3 treatment groups who showed progression of radiographic scores despite being in clinical remission throughout the second year, as depicted in the probability plots in Figure 2B. When we analyzed whether expanding the duration of remission into the first treatment year would have an effect on radiographic changes in the second year, we found that, indeed, a proportion of patients in whom joint damage progressed during the second year had attained their state of remission only shortly, i.e., ≤3 months, before the year 1 radiograph was obtained. This also translated into progression of radiographic scores at the group level. In contrast, in 80% of patients who had already achieved remission for 9 months before the first radiograph was assessed, joint destruction did not progress, and in the remainder of patients, maximal progression was numerically lower than that in those with shorter periods of remission. Therefore, joint damage in RA does not progress in states of sustained remission in the majority of patients. However, to fully confirm this fact, remission has to be present for a prolonged period of time before the first radiograph is obtained. Thus, we were able to show that preceding disease activity is a relevant determinant for radiographic progression between 2 time points.
Several explanations for this finding could be considered. One explanation would be that disease activity was misclassified and, rather than remission, low disease activity prevailed during the observation period, at least in some patients. However, this is unlikely, since among patients receiving MTX monotherapy, joint damage was halted only in those whose disease was in longstanding remission; if remission had been misclassified in these patients, the halt in progression would not have occurred, given their progression of joint damage during low disease activity. It might, however, be the case that subclinical joint inflammation prevails for an additional period of time after clinical remission has been achieved (20), leading to smouldering progression of damage; in this case, the lag time observed in our study would be overestimated.
As another explanation, joint damage could be an event that is totally separate from inflammation, at least in a subset of RA patients. However, this would not explain the results presented, particularly the difference between shorter- and longer-term remission. Moreover, in light of the compelling information on the effects of cytokines involved in RA pathogenesis (35–37) as well as the association of disease activity with joint damage in RA, it is unlikely that induction of joint destruction can be completely separated from the processes of inflammation.
Yet another explanation for our findings could be methodologic in nature, in that joint damage may need a certain amount of time to become visible by radiographic assessment. Indirect evidence for this hypothesis stems from data obtained using other imaging techniques, especially magnetic resonance imaging (MRI). Several authors have suggested that joint damage can be seen much earlier by MRI than radiologically (20, 38). Thus, any identification of joint damage in the course of remission would be the consequence of such a lag period in detection.
Finally, our findings could be related to the biology of joint destruction. In an experimental model of arthritis, joint damage identified by histology did not concur with the development of osteoclasts, since the evolution of erosions takes more time (23); this has also been observed in clinical practice (21, 22). Conversely, stopping the function of osteoclasts, once they have been activated, may require a longer time than would the reversal of inflammation. Regardless of the underlying mechanism, our finding of reduced joint damage progression in patients with lower disease activity before the baseline radiograph was assessed supports the hypothesis that joint destruction, at least as detected by traditional radiographs, is subject to a carry-over effect.
In summary, sustained remission is associated with a halt of joint damage irrespective of the type of therapy. The shorter the period of remission, the more likely some mild progression may be found, and this is likely a consequence of a carry-over effect of past periods of inflammation. Thus, sustained remission is the ultimate goal to prevent the occurrence of joint destruction and, consequently, the accrual of irreversible disability in RA. Moreover, in the process of therapeutic decision-making, the assessment of radiographic progression of joint damage will have to account for these observations regarding the latency of radiographic manifestations in patients with RA.”
http://onlinelibrary.wiley.com/doi/10.1002/art.24433/full
Yes, Kelly; RA does exist even in the absence of visible swelling.
Squeeze tenderness involving the hand joints (MCPs) & feet joints (midtarsal joints) has been advocated to pick up (in fact, not to miss) the early RA. One can always confirm whether there is any synovitis (actual swelling in the joints) with an ultrasound or a MRI.
Even patients who seem to be doing well will require adjustment of DMARD doses if they complain of pain & also have squeeze tenderness of the MCPs/ MT joints. If in doubt, one can always get ultrasound/ MRI done but not deny RA activity without confirmation.
doctorakerkar,
I am fortunate to have a rheumatologist who is sensitive to subtle changes in my joints which look fairly nice from the outside. She used ultrasound to confirm inflammation upon our first visit AND the beginnings of bone erosion. During our exams, if I say it hurts even a little, she takes my word for it and documents that in my record. It’s good to hear that she is not alone in her responsiveness to patients. Thank you.
Lisa
You are blessed with a good Rheumie, Lisa.
Something that I was always taught by my teacher… listen to the patients & the joints; examine, convince yourself & ONLY THEN have a look at the reports.
I am thankful to my teacher Prof. Dr. L. S. BIchile for that.
Doctor, may you have much influence in rheumatology with regard to this. Thank you for treating patients the way you would want your own wife, mother, or child to be treated: as fellow human beings who only want to get good care and get well.
Interesting that you mention the squeeze test. The last time I saw my rheumy and said how much better I felt after being on the plaquenil, less pain and stiffness, better movement, less swelling, during the exam he gave a gentle squeeze to a hand and a foot. Both caused pain. (I do try to avoid those firm hand shakers these days!) And so, in spite of no visible swelling and a good response to the plaquenil he suggested that I consider adding MTX, especially since I continue to have flares.
I think I have lucked into a very good doctor. I’m curious, how many of your doctors ever use a squeeze test for tenderness? I guess I thought that because my fingers felt so much better they were not really very tender any more. He really proved otherwise to both me and himself. Although what I am hearing more of here is about convincing the doctor about the pain you already know you have. This doctor has never questioned my reported pain.
My last rheumy was constantly underplaying my symptoms and telling me I was just getting older and I couldn’t have inflammatory arthritis because my bloodwork was normal. For the longest time I tried to go with him. He had a good reputation. He had the right training and certification. He was supposed to know how to treat me. But in my heart it just didn’t feel right. It didn’t feel like he was listening to me or my symptoms so finally I stopped trusting that he knew best and went looking for a second opinion. Best decision I ever made!
Leslie, it sure was a good decision. It can be scary to look for a new doctor because you aren’t sure you will find one who will treat you better. There are many rheumatologists who practice like your last one (I’ve met some), but there are also well-trained ones like the one you have now. Does make a big difference, doesn’t it?
You ask the key question: What percent of docs do this proper examination? What percent go just by labs like your previous doc? The only way to know is to poll patients who have actually been in the clinic with them. I hope Dr. Akerkar will answer, but he is in India, where there is also a shortage of rheum docs.
The first appointment with my last doctor, doc did the squeeze test on numerous joints and it was the first time I’d ever had my joints examined. Every other dr had just looked at the joints from across the room or gave them a tug to prove they could move passively. As a result of that exam, there was swelling and inflammation recorded in my chart in every joint that was examined.
Thumbs up to your new Rheumie. That is what good, aggressive rheumatology all about.
At the end of the day, it translates into good results & better prognosis for the RAers.
Kelly,
If I could I would hop a plane just to kiss U 4 this! I am printing and taking the article to my next app. Thank U. Susane & Mary, thank U guys too. Erica, I just had an experience close to yours. I asked about options after he admited that I have cervical spondylosis, and he told me I was not that bad, that he wished he could bring in someone really bad and show me bla bla bla. I got upset. I’m not a complainer but I have a right to discuss my health options with my Dr. i don’t want top hear from him that I’m ‘not that bad’ I am asking can I be better, is there something we can do? tell me what’s wrong with that. If I had not insisted that I was in pain regardless of taking the ‘majic’ meds, I would not even have gotten the xray that proved I was telling the truth. Honestly, I did not plan to go there today, I planned to be upbeat + positive. When I hear your stories though, I’m tempted to lick (hit) somebody down for the emotional and other harm they cause ppl who are already in pain.
Anyway, keep the faith folks.
God Bless
I wish you could come too Nicole. I could use that xo! Be sure to print the orginal study too. Amazing how many of us have similar experences once we start talking about it. I never had one say the part about “showing you someone really bad” though – but they have insisted that I’m not sick, not in pain, or don’t have RA.
It’s ironic that we choose carefully what to share with them and keep the most of it too ourselves and yet when we ask about options, our problems are minimized.
This whole conversation is very relevant to where I am with this crazy disease. About three months ago, I woke up and could barely get out of bed. The pain was horrible, out of this world, unexplainable. Just weeks before I had noticed a lump on one of my knuckles with mild pain in my hands. I made an appointment with my doctor. I hadn’t even gotten to the appointment when this happened. Needless to say I got in right away, and the blood tests began. The blood tests showed positive low RF and positive lupus anticoagulant antibody, which can be common in people with autoimmune diseases. A referral to the Rheumatologist, who ran his own tests and saw very little swelling was not impressed with my symptoms. His blood tests showed normal inflammation results. After another appointment where I was in great pain and another lump on my ankle; he asked if I wanted to try Plaquenil. Two weeks later I ended up in the ER with a mean, red, swollen hand, wrist, and going up my arm. They said that I had to stay and admitted me. There
Sorry! it sent in without me finishing. There was not any infection in my hand/wrist/arm. I asked the doctor why is this happening?? He said you either have a bad infection, or rheumatoid arthritis, and we can’t find any infection. I was there for 2 days. They put me on prednisone, and it helped a lot, but when I weaned down the symptoms all came back, so I went to the Rheum doctor again today. He is still skeptical that this is rheumatoid arthritis, because my hands are not typically swollen (as he put it). He asked me what I wanted to do? Did I want to go back on the steroids at a low dose. He is not ready to diagnose me yet, oh and by the way he tells me while I was in the hospital; my CRP level was elevated, but hands just are not swollen enough. I am so frustrated. My grandmother was in a wheelchair from this disease, and I can’ t seem to get the help I need, even with all my symptoms. Thank you Kelly for this forum. At least I know I am not the only one, but today when I left the doctors in tears; I did feel very alone trying to fight this disease. Thank you for listening. Deb Delaney
“Not swollen enough”?? I would probably get a second opinion, considering all your symptoms and family history.
You are NOT the only one who leaves in tears – I hear it from many people. I’m sorry you feel alone – it makes it even worse.
Thank you for the response, and this site. I come here and feel better to be with people who know, and understand. I tried to get a new referral when I was in the hospital. I would have to see another doc in the same office. It is the only office with the hospital where my insurance is.
Dear Debbie,
Sorry to hear about your story. If reports is what your Doctor wants, please discuss anti- CCP antibody & an ultrasound of multiple joints with him.
Dr. Akerkar,
I have had 3 of those type docs tell me that anti-ccp doesn’t matter at all, only CRP or ESR (sed rate). The anti-ccp was always >250 when they claimed I did not have RA or that I was in remission due to low “inflammatory indicators.” It was a lot of work to figure out why every joint hurt and I am so disabled when rheum doctors told me I was fine. That is why I’ve given my life to helping other patients find accurate information and be encouraged to fight.
I wonder what the percentage is of doctors like this, since most patients I know have met some of them. What is your best recommendation to patients who find such good rheum doctors? What do you think would help improve rheumatology education so that this would not happen? These errors delay treatment for months or years and I know you believe in early treatment.
A Rheumatoid factor may fool one but Anti CCP can only rarely fool when it comes to diagnosing RA.
Recent studies have even shown that if one has vague joint pain & the anti CCP is positive, the person needs close observation as he/ she would evolve into full fledged RA sometime later (Anti CCP predates the clinical manifestations).
Health care social media has been a very good eye opener for me in recent times. It give me the patient’s perspective; the story on the other side of the table. It has helped me improve on many counts.
Take this voice of RAers to such heights that it falls all the Rheumie’s ears. It’ll tell them what books dont. RAers should be promoting the good Rheumies they have met.
Wasting time in diagnosing inflammatory arthritis is criminal as the time wasted is function lost in the long run…
Hi Dr. Akerkar
Thank you for your response. They have done a lot of blood work since this started, 14 weeks ago. The only ones that are positive are low rheumatoid factor, lupus anticoagulant antibody, and CRP. These are the tests they have told me about. I have heard here on this site that one should get copies of their blood work; I am going to do that this week. I will have to ask about the other tests you have mentioned. I am 48 years old and working on my MA in education, and special education, this illness has me thinking about quitting school. The symptoms of this illness have been severe. It has affected my wrists, hands, feet, ankles, and shoulders (both sides). It has started to hurt, and swell one knee also. The weakness and pain are so bad some days; I have trouble walking, or lifting something as light as a coffee cup to my mouth. I have had trouble opening doors; my husband had to change our front door knob to a lever knob. It was becoming dangerous not being able to open my front door, what if there was a fire. I have has days where I can’t move the blankets off of me to try and get out of bed! I think that this is the reason that people try and get help so badly. Their whole life changes and then people I have read about here are waiting years for diagnosis and treatment. Early treatment is supposed to be very important, but how can you get treatment if you are not diagnosed? I feel so bad for everyone. My grandmother had rheumatoid (they called it crippling arthritis), and she was in a wheelchair. The doctor used to come to our house and give her gold shots. That was many years ago, and today people are still having trouble getting help for this disease. I would not have known if it didn’t strike me, and I did not find this site. You are helping many people by responding on this site. Thank you! It is good to know there are doctors like you helping others. Best wishes to you.
Deb Delaney
reading your blogs on your website has me evern more uneasy than i was last week…….i will explain why.
I was in the Navy for 10 years and I was exteremly active, running 3 1/2 miles every other day….playing volleyball, basketball, and softball, and i was lifting weight because i was only 108 pounds. I five years in i had a five year physical and was cleared to move to Japan for my next assignment. After being in Japan for three or four months i was haveing trouble with my lower back and my legs from my waist going numb after sitting for more than 10 minutes. 🙁 i was an administrator so my Job was sitting at a computer/desk and acking stuff to send to the states.
i went and saw the newest “Dr” in the Hospital and he sent me to physical therapy to learn how to sit move and lift things in my daily life, even though if you were to look at me there is a lttle girl who is too small to fit in the smallest uniforms. I was 24 at the time….but was confused for 16. 🙁
anyways i went to the class sat thru the boring slide show that i have seen at least twice a year for the last 5 years. then we were taken to a room with floor mats and was shown how to stretch to help our backs and so i am on all fours streaching like a cat and i was told to stop….the instructor was across the room from me and he jumped over a couple people and told me i needed to get up and wait in the other room till he was done with the rest of the group. 🙁
He told me that i need to see an otrhropedic surgyen and he would call to see if he could get me an appointment with that Dr. adn in the mean time i was the head of PT and she confirmed and sent a referral with me down the the ortho dr.
Is i ended up having scolois (sorry to this day i still can not spell it) and he told me thatI am still young so it shouldn’t bother me and that i am no longer growing and it shouldn’t progress and more than the 30 degreese he found it at. He would do more xrays to check it in six months. but he could not explain my pain and numbness. In three months i had progresses to 31 degrees and i was sent to a specialist in Okanowa and he came in the room and looked at me and said there is nothing wrong with me then he looked at my xrays and a little Japanese man came in and made a brace for my back and the Dr came in and said that i was to see a Dr at walter reed and have surgy done to help me.
I was at WR and the Dr there told me i am too oung and it is very mild so there is nothing he will do. I asked him about my pain and he told me it is in my head. 🙁 at this point i am no longer running, I am barely walking to my desk to work and to my car then home. 🙁
so i have going to PT and Drs for the last few years and getting no releif for the pain. I had my first child in 2005 and then i was in the building at work and fell down the stairs…i had three officers behind me i was so embarressed that i didn’t assess my pain. then i had to take personel records back and was going up the same stairs and once again fell….with the same officers behind me again…..now i am in working whites and the stairs have the black no skid paper attached to them!! i was more afraid i made a hole in my pant in the seat and knees than i was about my pain i got to the building that had no elevators but where i had to go had three flights of stairs and yes i fell going up and down each flight. a few weeks later i started to fall walking on flat surfaces and it was found that had a laberal tear. I had surgry in May 2006. I was doing good. 🙂
then it was time for me to start my sepration physical…and i guess i passed and the Dr signed my paperwork and sent me on my way…..a couple weeks later i was not feeling the greatest so i went to general medicine and the Dr that i saw there pulled my info on the screen and started to turn red. 🙁 she asked me all of these questions like do your hands swell and hurt? how about your knees and feet? adn she was poking me and asking me if it hurt….i thought she lost it i had the flu or so i thought and here she was poking me……i was having trouble sitting in the chair because i was trying to keep the little bit of water in…..then she asked me if i was told to call a Rhuematologist…..and i asked her why….and she said in my blood work for my seperation and i had a high RF and i needed to get checked out very soon. she got up and went to another office and cursed out the dr that passed me in my physical and not informing me about the RF. she came back and called the RA dr and then i was walking out her door to the RA floor. 🙁
i got an appointment for the next week then gave blood for the next week and that weekend i was in the ER cuz i was so sick…..and i found out that i was pregant with my second child. When i met the new Dr he told me COngratulations and i do have RA but there is nothing we can do until you have your baby, and if you don’t have Lupus during this pregancy you will after it. at that time my ANA was 640:1 and stayed that high till i had my daughter. three weeks after i had her it went normal. now she is four and my Ana was at 1280:1 five months ago. I have not had bloodwork done since that one. 🙁
My RA doctor has told me that i do not have RA but i am borderline bothe RA and Lupus and then six months ago she told me as a secondary i have Fibromayga. 🙁
I have a six year old and a four year old and my RA dr moved to Hawaii. I am stuck i need to find a new Dr but so far my experiences with Dr are extreme from telling me there is nothing wrong to starting me on everything and letting me swim or sink for three months on my own. 🙁
I am tired i hurt and i need help cuz i have no clue what to do. Can you please help me? Your blog has helped me that last couple days i have been reading i and i wanted to thank you for that but i know i need lots of help! 🙂
Wow!! I am dealing with this exact problem! I have recently had to switch Rheumy because of lack of insurance and in seeing her for the first time last week, she also suggested that there was no swelling, just be looking at the tops of my hands! I have all other symptoms and I have been on RA drugs for many years…Why are these doctors not taking us seriously?? Meanwhile, I am only on pain meds because this new doctor believes that since there is “no swelling” than I do not need any RA drugs!! What do I do??
Sounds very familiar, Melissa…
I can’t tell you what to do, but if you’ve had RA diagnosis and treatment for many years and the new doc only offers pain meds, that does not sound right. I have heard this story before – and lived through it – so I wish there were a better solution! Read Ann’s story in the RA story pages and I think you’ll nod your head.
I guess trying again for another doc is all you can do. I’m very sorry you have to go through this, but I’m right there with you.
My rheum continues to treat me with mxt, enbrel and pred… And continues to say that my RA is atypical due to my labs tests which are all negative, but my inflammation is always so apparent and already have deformity with just 6 months of RA. I have had very little diagnostic studies performed (just xray prior to my dx which showed some bone erosion). My rheums assessments are very poor with every visit which I find very dissatisfying and I am lucky if he looks at my swelling. Still, I try not to complain about my rheum lack of attentivness as I doubt it would make little difference in my treatment since I am recieving a
Dmard and biologic to try and halt my disease progression even with my sero neg diagnosis.
It appears that with the general consensus, I am lucky to get that much! Isnt that just so wrong? I am frightened to seek for another rheum just on the basis for a more detailed assessment, due to the fear that the new rheum will attempt to tell me I do NOT have RA, that there is nothing wrong with me, and that I do not require treatment. With everything I read, who could blame me for being scared?
I just want to be healthy and to be able to chase after my children. I want a doctor that I can trust who will touch my joints. Obviously thats too much to ask for?
If you are afraid, I’d recommend keeping your current doctor even if you ask around for a new doctor. You don’t need to actually make a switch until you have found a doctor who is better. Going to ask for a second opinion should not be a problem. I know it often is hard, but I’m just saying I wish it weren’t that way.
As far as whether being treated with medicine is enough, that is a fantastic question. And I am writing about it this week for another post in this series.
No Aimee, that is not too much to ask for. Get as good care as you can.
I look forward to your next blog kelly! Thank you Dr A for your so valuable input!
Wonderful Blog Post! I rarely have swelling that is obvious and only have had an elevated SED Rate and CRP but I am negative RF Factor and Negative For Anti-CCP…I have pain and some swelling of the Wrists, Ankles, Knees and Knuckle Joints…but have pain not only in the joints mentioned but also my shoulders, hips and feet as well…Early on it was very difficult for Rheum Docs to want to treat my disease with anything other than Plaquenil and NSAIDS. But soon my SED rate started to climb and the CRP became elevated and my quality of life was slipping away…I now am finally on Humira, Methotrexate and 10 Prednisone (for now anyway), in order to function without a great deal of pain. Now I can walk, go to the store and I have even started swimming in my local pool! I am taking it slow but I am starting to see progress. I wish there were more Rheum Docs like Dr. A…I have had MD’s tell me that I could not have RA because I did not have inflammation markers that were high enough, I was told that there was no swelling, therefore I had no disease…(without an exam!) I was also told that I could not have RA because I was RF negative…which we all know is totally false…At least now I have a Rhuem Doc that will actually treat me! Thanks to Kelly for more discussion about RA and Swelling Part 2!
Thank you for addressing anti-ccp and thanks Kelly for such a great discussion and blog. So far I am positive anti-ccp and negative for other bloodwork but Dr keeps thinking early RA. Went to 1st Rheu. appt last month, he thinks probably not RA but did neck, spine and hip xrays last week and I’m to see him in September. If it is RA I havent heard how early any medication should be started to stop any possible damage and if a positive anti-ccp has ever gone on to be something else. Everything I read says the test is pretty specific for RA.
We have talked about anti-ccp quite a lot and adovocated for it to be used by primary docs instead of Rheumatoid factor to screen for early RA. Not all RA patients are ccp antibody positive,but the test is very specific so if you are positive, it’s an extremely strong indicator (probably about 95%) that a person has or will have RA symptoms.
September is a long way off in the context of “early” treatment. I hope you can get an answer sooner than that, Marla. Look at the Tag for Tests if you want to find more posts on the topic.
kelly, from your research and contact with other raers, have you found it to be very abnormal to have RA and a negative anti ccp?
Dear Aimee,
There are patients with RA despite a negative anti CCP report. This is a minor group though. What is very odd in your case is the rapidity of progression of your RA. This is odd with a negative anti CCP as we equate anti CCP with rapid progression & poor prognosis.
The other causes in patients with early inflammation in joints & a negative anti CCP test would include evolving SLE. The arthritis component of SLE may be the first sign of SLE in these patients.
Technically, early inflammatory arthritis with a negative anti CCP test is labelled as Undifferentiated inflammatory arthritis. Methotrexate has been shown to be an effective agent in this case too.
You may know more about anti CCP here (http://www.arthritissupportboard.com/Anti_CCP_antibody_in_rheumatoid_arthitis.aspx)
Thank you Doctor. My Rheumatologist did mention that I could possibly have undifferentiated inflammatory arthritis which he explained to be another subtype of RA. I am being treated on 20 mg Methotexate and Enbrel currently but have not found any relief yet aside from prednisone which helps mask some of my symptoms and decrease the systemic inflammation (high temp and rash). I have tried Humira but I sadly did not respond to it. I will ask my doctor about SLE when I see him, I don’t think I have been tested for SLE. Thanks so much for the link and it is so wonderful to get your very valuable input, I so appreciate it!!!
Aimee 🙂
After reading everyone’s comments, I actually feel “good” about having both ankles swollen, both knees swollen, 1 finger balloon-shaped and no strength in both hands, as my Rheumy doesn’t question whether I have RA.
This disease is one where it is difficult to fight back as we are just too tired. I am one of the “lucky” ones. My Rheumy does listen. He looks at my joints each time I go and does a diganostic questionaire about how I’m doing on a scale from one to ten. I can still go to work each day for the most part, although there are days I just want to hid under the covers. Right now my SED and CRP levels are dropping to almost normal, but I still have pain, and am losing weight, even when my swelling is minimal. This is one strange disease. It makes me wonder if it is similar to Herpes and hides out only to jump out when least expected. Someday they will figure this out, or at least I hope so.
I hope so too Meg. Listening to patients like your doctor does will be a huge step in that direction. Weight loss and pain are signs the disease is active of course even though your labs look better. I’m glad he realizes that.
Sarcastic comment here,,,,,Don’t Doctors have medical PRACTICES? …Yes they do…. & they are practicing on us.. So they don’t know it all & should be receptive to learning something new every day of their lives like we all do as we live this life. This disease does what it wants, when it wants & how it wants to each person. We are all different & should be treated as individuals not typically.
Good one Cyndi, I couldn’t agree more! “This disease does what it wants, when it wants & how it wants to each person. We are all different & should be treated as individuals not typically”.
They may not have met my RA before, or yours!
I would say nice to have company but I’m sorry we all have this disease in common. RA sucks, just that simple. And not having a DR that listens and understands is as bad or worse. I am being treated at a VA hospital and while I am very thankful for the care, my dr is about to be replaced. Need pain meds, not up to him, have to see your Primary care. Okay, can deal with that. Ankles, feet and lower legs swelling? Does it hurt to move your ankle…not at this moment…then not RA and not his problem. I guess he never thought that it might be from any of the meds he has me on. I think it is from lowering my Pred from 10 to 7.5. MTX not working? How could that be??? I just took my MTX last evening, today I am having hand, elbow, knees, toes and ankle pain. And swelling in all mentioned. I apologize for the sarcasm, but it gets so frustrating. I used to be a very healthy person, rarely getting sick. Now I have had three infections since I started on the MTX in Jan. Gone from taking no meds to 7 different pills a day not including the 20 mg of MTX a week. But after reading these posts, I realize I am lucky I am getting treatment. Also I had to nod my head often reading some of the posts, been there. If you haven’t experienced the pain of lifting a glass to drink out of or trying to pull your blanket up while in bed, unbelievable for such a simple task to hurt so much. You just sit and cry. Bottom line, I am not a doctor but I will arm myself with all of the knowledge that I can. This is my life and my body. I refuse to tell a dr that his treatment plan is working when it is not. Sorry.
Hi All, Like most of you I usually have little swelling (only my left knee, which has been that way since I was 13, I’m now 33 yrs old). I am currently having the worse Ra flare that I have ever had, and I have had it for 5 months now 🙁 This week I have been running a low temp between 99-100, does anyone else have this problem? I have never ran one before, I usually run about 97 so this is kinda strange for me. We changed meds from Embrel to Humira about 3 months ago and I am wondering if that has anything to do with it. Any other suggestions to help me would be great, tired of being tired, and thankful that I have a great family that someday I would like to get off the couch to spend time with again. Hope everyone else is well 🙂
Megan,I have ongoing low grade fever with RA, many do. It has been a year since It started. I switched from Enbrel to Humira because of the fever and increased pain. It seemed to work for a short time, but hasn’t done anything for awhile. The Enbrel did the same thing. I can keep my fever down to 99.3 and below with prednisone 7.5-10mg. Otherwise it would go to 100 with activity. I just quit the Humira, my last shot was almost 4 weeks ago. I don’t feel any change from missing the humira, so I don’t think it did anything. Be sure to talk to your doctor about the fever and flare. Coincidentally, my first joint to swell was my left knee. The doc, drew the excess fluid out and gave me a steroid injection-huge relief! Methotrexate seems to keep my inflammation from going crazy too.
I am so unbelievably happy about this post! I have been trying to tell my Rheumy about my wrist and he never would believe me. I just wonder if I print out this article would he think twice or am I really going to have to find a Rheumy that will get this….Why don’t Doctor’s ever listen to you.. I’ve had 5 surgeries. 2 of them wouldn’t have had to happen had the doctor listen to me early on. Thyroid and Gallbladder. 20 yrs of telling him something is wrong with gallbladder and 10 to 15 yrs about the fatigue a telling him to do the more intense testing,that was unfortunately done in the latter and me working at a Radiology center. Seriously ignorant of us as patients!!!
Hi, I was diagnosed with RA in August 2008, and let me tell you, I have not had a good day ever (at least it feels that way). My ankles both swell to the size of grapefruits, meaning when it isn’t flip flop season, I have trouble with shoes and socks.
My Dr tells me I have a very aggressive and progressive form of the disease. I am only 30, but he says that my disease is acting as if I’ve had it for many, many years. I have been on Humira and MTX for almost 2 years now and the Humira has stopped working. The Humira did work for a while, my swelling wasn’t very bad, not as bad as it is now, but I was able to tell when it was slowly not working for me, and so he switched me to Simponi, but that landed me in the ER for nine hours with a 104 degree temp and just horribleness all over, and so after that nice scare (this last January), he told me to stay off the Humira and just keep taking the mtx and arava, and now he wants to put me back on plaquenil, hoping that along with the other two (and maybe enbrel) will keep my swelling at bay, but I can’t afford the plaquenil right now so I am waiting to get it through the Sanofi patient assistance program, I get most of my expensive meds through the programs, because I am on disability and have no current insurance.
But my Dr is wonderful. He examines you thoroughly, poking, prodding, squeezing, testing my grip strength, my joint flexibility, even if he is running late on his appts he still takes the time to examine and talk to you. I am glad I found him the first time around and haven’t had to shop for drs. In a way, the swelling is painful and makes life a living h e double hockey sticks, but at least it makes the disease visible. I hope you can find and keep a dr that you trust and like. I would never go to a dr that makes me feel like a burden to him, or that it’s all in my head, or that I am overweight therefor must be lazy. The only thing that reduces my swelling is a high high dose of prednisone, and I have gained almost 100 lbs in two years from that drug. I can’t exercise properly because I have a pinched nerve in my lower back that limits my walking capability. I can barely walk 2 blocks w/o having to sit because my leg is either too numb and weak or too painful to go on. But I cannot afford to get the nerve fixed until I can get insurance, so my exercising ability is limited. Prednisone is a great drug with horrible side effects.
And I don’t know about you, but RA has become not just RA for me, it’s become Fibromyalgia, a touch of sjorgren’s syndrome (my skin, mouth, eyes, most everyplace is constantly dry)….and etc. I’ve heard that once you get an autoimmune disease, you get others as you go.
Good luck.
ELN,
Look into the RxOutreach.com program which offers many generic medications at low fees. It is like an assistance program and there are income guidelines. But to be honest, income verification is never required. Plaquenil is included in their list for feeds of $25 for 90-day supply or $45 for 180-day supply. This program has helped me tremendously when I have exhausted my prescription coverage.
Lisa
I am so grateful for this and your previous post about swelling as well as all the responses. I am a thin woman and I see swelling where others can’t. There are times I have to wear larger shoes or cannot wear my rings. I had an ah-ha moment as I was reading the responses. The increase of pressure marks in my skin (lines from my pillow case, marks from a pair of socks, bra strap dents, etc) ARE SIGNS OF SWELLING. There have been 3 days in the last 3 months where my husband has been able to visually see swelling (and I took photos), though he notices the pressure marks all the time. Having times when my fingers, wrists, feet, whatever are larger (read: without sausage look) is indicative of swelling due to my RA.
Thank you for helping me develop an understanding of me!
Jenn
Jen, I was nodding as I read your post. I have terrible pressure marks like you describe all the time and it’s not fat – I have only LOST weight with RA. I can’t wear any of my shoes or rings from “before.”
I am nodding along with both of you on the subtle swelling and being thin. Although I have started to gain weight from MR.Preddy-sone, blah!
Unfortunately, I have Type 1.5 diabetes (at least 4 injections each day), high blood pressure, cholesterol, osteoporosis, osteoarthritis, and rhematoid arthritis. I would hate to tell you how many meds I take each day and how expensive some of the meds are. I’m sure we all have that same problem. So far, I am only on MTX and pain meds for the RA. I have a lot of drug allergies that limit what drugs I can take for the RA (allergic to sulfas, NSAIDS have done some stomach, kidney and liver damage, etc.). My rhemy just started increasing the MTX dosage but I am having trouble tolerating the new dosage (extreme fatigue for 4-5 days after taking and diarrhea). In other words, I have so many problems going on that it is very difficult to find a suitable treatment for me. My ankles are swollen and tight and really hurt. My fingers are swollen and stiff and hurt. My neck and shoulders also hurt. My whole body is stiff and feels like I am trying to move a 1,000 lb. object around. My opthamologist is treating me for severe dry eyes caused by the RA. Sometimes I just sit down and bawl because of the pain and the despair that I am feeling. It seems like I am never going to feel good again. I am calling my rheumy to let him know the MTX is not working. Hate to go on prednisone cause it really elevates blood glucose levels, but I am desperate enough now to okay a short term treatment. I hurt enough that I am ready to try the biologics. I was diagnosed 1 year ago, but I think I have had the disease a lot longer because my past doctors blamed diabetic neuropathy for a lot of my complaints. Between my primary care physician, my rheumatologist, my endocrinologist, my dentist, and my opthamologist, I have at least one medical appointment each week. I am sick of this MESS. However, even though my rhematologist has a bit of an attitude, at least he appears to be listening to me and trying to help me. I sure hope something clicks and starts working. I would like to see my ankle bones one more time. LOL. Thanks for letting me vent. Love and peace to all my fellow RA warriors.
AMEN SISTER! I ranted about the same on a comment on your last post!!
I am in clinical “remission”, but I DO have active synovitis,no dobut about it. My Rheumy knows it too.
Dr. Beynon always says that “well controlled” does not mean “well” or “normal”. Too right.
I too, have had swelling and Baker cysts in my knees.I know how you feel, and all they can do for you,sometimes would be: shots,draining, more or different meds! So, you wobble out of the docs office,really not feeling any better than when you went in,and maybe a little more sore due- to the shot and draining. RA is just horrible,really horrible.
after how long did you have that done? Mine have been “ignored” for so long, I wonder if they think it would do no good?
Thanks, now that you say that, when I’m active in the morning is when I get the fever in the afternoon 🙂 This flare up is the worst, I now have both my knees, some of my toes and fingers and for some reason my neck is acting up and giving me killer migraines 🙁 But as we all know, this is not fun 🙁 I have tried the steroid injections and they do not work on me, but I’m glad to hear they work for you 🙂 Luckly I have a wonderful Dr. here in Indy, if anyone needs one let me know, mine is awesome! 🙂 He really stays on top of my pain, I’m not your typical sweller, just lots of pain. I have never in 10 yrs had a test come back positive, I was digagonised through orthoscopic surgery (the Dr. was smart enough to take a sample of tissue and test it, thank you to him or I would have never been diagnosed). Hoping to go back on metho after my stomach problems go away, I’m hoping maybe that will help with the swelling. Hope everyone else is feeling better with the relief of warm weather 🙂
I think from what I’ve heard from patients, there is not a “typical sweller” anyway. Swelling seems to be highly variable. It’s so good to hear you have a good doctor who knows how to treat your RA. If you want to add his name to the recommended doctor’s list, you can email it to me. kelly @ rawarrior.com
Several people have mentioned being diagnosed during surgery.
Went to my every two month appointment with my DR. Good news, he is moving!!! Will see a new dr next time I go. Am praying that this dr doesn’t base my well being on if I have any major swelling going on. My wrists are already showing deformity and I have only been diagnosed since last July by symptoms. Didn’t get the formal diagnosis until Dec after an ultrasound. Oh, I am seronegative. This dr told me that since I don’t have any major deformities, my pain should be minimal and my level of RA is considered mild. Hmmm. Wish someone would tell my toes and feet that today, they are very unhappy!! Also told me headaches are not a side effect of MTX. And pleurisy is not a symptom. I did get mad about the last one and told him he was wrong. I have had pneumonia once with pleurisy in 2004, once you have had it, you never forget what that feels like. When I first got RA, I had pleurisy in the same side, knew right off what it was. Sure he is probably glad to be rid of me as well!
I am starting on Plaquenil, could not tolerate Sufasalazine. Hopefully this combo(with MTX) will help because I am going lower with the Predisone, down to 5mg. Have gained forty pounds since Sept. Thankfully I lost about 15 before they started me on steroids. Still, have Cushings…moon face, most of the weight in front, hump starting on back.
Don’t know about the rest of you but I really am not totally miserable until I try to do stuff, like vacume or clean, wiping a table can set it off pretty good in my wrists and hands. The fatigue is really tough to handle. Without a two hour nap, I am done by 7 or 8, in tears and nauseated by 9 if I have not been able to get in bed. What can you do? Trying to explain this to someone else, I don’t know, they look at you like – Well, you look okay. My family knows better, I have always been a very hard worker, a very physical worker. Like will put in a chain link fence and have fun doing it. Now I’m really not worth shooting. Couldn’t dig a post hole, that’s for sure. I hate this stuff!!
Thank you, thank you, thank you…finally, someone hears what I’ve been saying all along. Time to find a new Rheumy that listens and sees the whole person.
I too have been to my dr & have told him my hands, wrists & fingers have been swollen & tight. Finally, seeing me shortly after my Rituxan treatment when I did NOT have swelling, he realized that I really had had swelling before. I have very bony fingers and wrists so swollen for me doesn’t necessarily look typical, but definitely swollen. My point is that not everyone looks the same when swollen and that better documentation needs to be done when joints are looking more normal so a good comparison can be made. And if there is a tight and swollen feeling with documented RA without obvious swelling, how does that qualify as remission? Isn’t remission suppose to be pain & sympton free?
I agree that remission should be symptom-free or almost symptom free or at least pain free. And swelling varies so much and is so subjective, it is shocking that some keep pointing to it as their most reliable number to predict disease progression. It is completely subjective as a measure.
edit: by “number,” I meant swollen joint count (SJC).
P. S. Having read the previous posts I have to tell you that I also can no longer wear my rings because of swelling. Stretch rings are great.and cheap! So you can wear fun & fashionable and be comfortable! Have fun with them because with this miserable stuff we don’t get enough of that!
I’d also like to know why a patient’s word cannot be enough about swelling. If a patient says, “It does swell sometimes,” why do we have to show pictures to prove we told the truth? It’s starting to bother me – we already have a diagnosis. We don’t want to need medicine, but we do. I just don’t understand why seeing it swell first-hand is mandatory to some docs. NOT all. We all have heard comments from people with good docs who don’t require swelling for treatment. And I’ve met a couple of them.
My new Rheumy insisted that I don’t have RA because “the RA meds I have been taking are not working”. Therefore I “must have fibromyalgia”. All I can think of to say is aaaaaaaaaargh!
and how long have you had this disease? What did he say about your affected joints? (Haven’t I seen some pictures right?)
I am taking embrel for the last 10 yrs. & methortexrate for about 8. This last year I run about 102 temperature twice a month in the mornings. Does anyone else have this ? I think its from the meth. But my doc. doesn’t believe I even get the temp ???
Thank you for this post. I have had joint pain, swelling, red and hot joints, the skin feels tight around them and they’re stiff in the mornings. I had my first rheumatologist appointment yesterday, after waiting 3 months to see her. Unfortunately yesterday was a rare day when I was feeling ok (just my luck!). I didn’t have any swelling (like I usually do). Even though I’ve had 3 GPs see the swelling, my rheumatologist said ‘it doesn’t matter who’s seen the swelling, if I can’t see it I can’t do anything’. My GP put me on Prednisone because I couldn’t walk or hold a pen (and I was moving cities as well). The rheumatologist said ‘that was stupid, who ever put you on Prednisone shouldn’t have’…!! Was I just meant to hang out for 3 months not being able to walk, hold a pen/cutlery/open doors?
She ordered heaps of blood tests, but had a poor attitude and seemed really unsympathetic, not to mention she answered her pager and cellphone all throughout the appointment! My GP knows the rheumatologist and said that she often wonders why she’s a doctor because it’s clear she doesn’t enjoy her job.. I’ve got another appointment in 4 weeks, I’m hoping I have some swelling for her to see them. In the past my CRP, Sed Rate, Rheumatoid Factor, Anti-CCP have been normal, but elevated ANA.
I live in a smallish city in New Zealand so it’s not so easy to just find another rheumatologist. My GP said if the rheumatologist has the same attitude next time then she’ll try get me into see someone else.
Thanks for this article. I’m just so frustrated I couldn’t swell up like I usually do for her!
Oh, that’s a nice one: ” ‘it doesn’t matter who’s seen the swelling, if I can’t see it I can’t do anything’.”
Good luck Mary! I think I would have asked her, “What would you for me do if I swelled in front of you? Can we just try that?” Very curious.
Yes! I know, as you can imagine I was SUPER pleased to hear her with that attitude!
Thanks, I have a feeling if I got a bit lippy with her she would be very rude back!
I said to her ‘if you’d seen me last night, you would have seen something different’. She said ‘what would I have seen?’ and I said ‘ummm swollen knees..’. She asked me if my toes ever swelled, I said ‘I’m not sure, I don’t look at my toes often’ and said she ‘why not!?’ Lol well I wear these things on my feet… they’re called shoes!
Thanks for reply =]
What is the most stressful activity you do? For me and my hands, it is pulling weeds in my garden. Always makes my hands hurt and swell. So-play their damn game. Go do that thing that kills your hands (feet, wrists, elbows, etc) the day before the visit and go into the office with claws instead of hands. I admit I have done this because I wanted the rheumy to SEE FOR HIMSELF what I deal with more days than not. Some other things that make my hands respond, in case you need an idea-scrubbing the bathroom/kitchen with a nylon scrubee and Barkeepers Friend, washing fine clothes by hand and wringing them, even lightly, out, polishing a piece of furniture or washing windows. Just my 2 cents worth.
I’ll think more about what you said Susan – I like your logic & strategy for those stuck wtih wrong minded doctors.
Those are all things I haven’t done in 5 years – since the RA found my fingers. In trying to guard against deformity, I’ve avoided all behavior that causes them great pain or anything listed in joint protection articles I’ve read (such as any wringing motion).
I haven’t been able to wash dishes since 05 & I did try to pull weeds a few times back in 06 but I could not pull the weeds, only pulled fingers out of position when I tried – the weeds did not budge. I had been a very active gardener before that. Do the weeds actually come out? I would like to read your answer – an upcoming post may have a clue about this – working on something.
I know it is a terrible logic. A nurse actually suggested it in a very subtle way. Yes, I can pull the weeds but I truly pay for it later. I love gardening. It is part of my sanity plan. There are just some things I do in spite of the RA. And yes, the wringing motion is one that everyone tells you to avoid. I have even used a shovel a few times to highlight the multi-joint involvement. Now the RA is in my toes and ‘knuckles’ of my toes and they show up as scarlet and fat. I hate the idea of deception of any kind but dang it! I know I am not faking!!!!!!!
I was diagnosed with moderate to aggressive RA in March of 2011. It has been crazy ever since! We have quickly advanced to infusions as nothing else seems to work, I start next Monday. I have reactions to almost everything. I can’t take any of the sulfur based drugs. My methotrexate injection makes me nauseous. I switched to bedtime, I still feel sick the next day.
I have severe swelling. It started in my legs, which was odd. Odd, because it was my shin to the back of leg, only the outside of my leg. My doc did x-rays but explained it was a symptom of MY RA. Now the swelling is in my both legs and my arms swell so I can only wear sleeveless shirts usually 2 sizes too big. The swelling comes and goes. It is painful when it’s excessive.
I am so glad I found this site. I tire of trying to explain the pain. My kids, adult and out of the house, want me to quit work and stay at home. It’s hard to explain although I am in constant pain I have to keep moving. I encourage all my family and friends to read your site. My husband has found it very helpful. He sometimes points out new symptoms to me that read about. I will mention it to him and he will say that’s your RA, I saw it on the site.
I believe I have a very good doctor. She is being aggressive. When she changes or adds a rx she allows the allotted time for it to work. If it doesn’t, she goes to the next treatment. She admits we have to find the right combination for me. She also encourages research.
Thanks again for all the posts!
My mother (deceased now) and I both have severe rheumatoid arthritis. Mother’s hands were horribly painful. They were so misshapen they appeared to look like paws. Mother had gigantic lumps on her fingers and wrists. I have never had much visual swelling. By the time I would ice a painful joint and go to the doctor, they couldn’t detect any swelling and I would get dismissed with a shrug. Only on Xray, could you see my RH damage. It took me 15 years to get an accurate diagnosis because I didn’t have the classic swelling and lumps. I was so deformed and had had so many joint surgeries that I could hardly walk any longer. Still, no swelling to confirm the diagnosis until 2011!