RA Surgery — 10 Questions Answered
This week I had my second RA surgery, after 13 years of living with severe, unrelenting rheumatoid disease that does not respond to medications other than steroids. I definitely asked my surgeon lots of questions. But, this second time, I knew even better what to expect by what I had learned last time. I hope these Q and A help you decide and prepare if you need RA surgery.
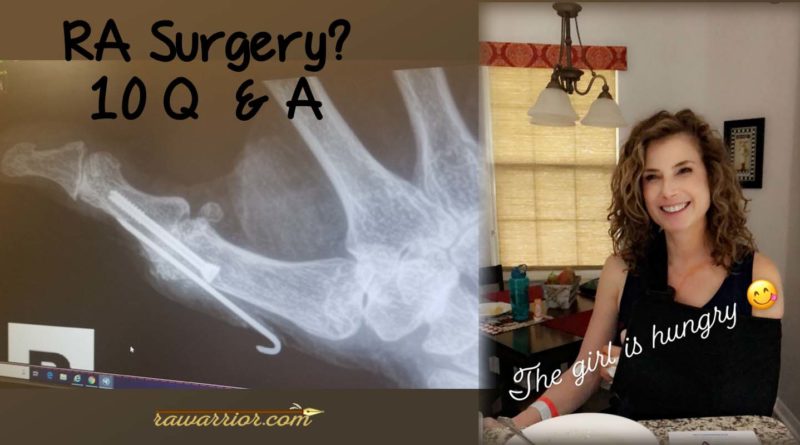
The two RA surgeries this week on my left hand (yes, I’m left-handed): fusion of MP thumb joint (the middle joint of the thumb) and trigger finger release of the middle finger. That’s the one that causes my hand to stay locked into a paw-like position. The surgeon said he actually cleaned out a large amount rheumatoid gunk from my finger.
Before RA surgery
1. Should I get RA surgery now or should I wait?
Only you can decide. My hand / shoulder orthopedist always says, “You’re the captain of this ship.” Generally, he’s very conservative, meaning he waits until surgery is the only option left. He says he really likes my willingness to try everything I can and avoid surgery as much as possible. My knee / hip ortho doc also leaves it up to the patient.
2. Do I stop RA medications for RA surgery?
The disease treatments used in RD / RA reduce immune function, so some doctors pause those DMARDs around the surgery time. They worry that the medications could slow healing. However, I have seen several reports in recent years showing DMARDs can be continued with RA surgery. Stopping DMARDs carries a risk of losing treatment response—DMARDs may not work the same after re-starting.
My only RD / RA medication is steroids (shots and prednisone). I could not have a shot in that hand during the weeks prior to surgery, but otherwise, my medications continued.
After RA surgery
3. How bad does RA surgery hurt?
This will depend on what you have done, but all surgery creates a wound that can be painful. For me, the pain after hand surgery—including inserting titanium screws into the bones—has not been as severe as my RD / RA pain when it is bad. The surgical staff and the anesthesiologist worked hard to keep me comfortable. As the nerve block wore off, my hand hurt; but two days later, it only hurts when I accidentally use it too much. On the other hand, a total joint replacement could obviously hurt for a longer time.
4. How much will RA surgery help?
This is the hardest question—even your doctor can’t promise an answer. Most of the time, a fusion or synovectomy or arthroscopy can bring a good amount of pain relief. But my doctor repeatedly told me two things:
a) “I’m only fixing one joint—all of your other joints still have RA.” It’s true and it seems strange to fix 2 joints out of 200 that need help.
b) “We cannot promise improved function. RA surgery is focused mainly on pain relief.” Of course I can hope for both.
5. Do joints look better after RA surgery?
In addition to pain relief and better function, this would be nice, wouldn’t it? I have looked at surgery photos where badly bent toes or fingers look straighter after surgeries like fusion or joint replacement. But appearance is another thing that my surgeon said he could not guarantee.

Preparing for RA surgery
6. Is there any reason to avoid surgery?
Even after deciding that RA surgery is a good option, there is still your overall health and disease progression to consider. Your surgeon should be informed about all aspects of your health and the ways RD affects you. This will give her / him a good idea of how well you can handle the surgery and heal afterwards.
If you have very active rheumatoid disease, it will continue to progress despite surgery. This is actually the reason my surgeon has not cleaned up my shoulders: he says that by the time they healed, nasty rheumatoid effects would begin to build up again in those same joints.
7. Who will do your RA surgery?
RA surgery is performed by an orthopedic surgeon—preferably one who has done many operations on people with rheumatoid disease. If you do not know of a good one in your area, be sure to read several online reviews from her / his patients. None of the rheumatologists that I’ve seen have ever mentioned surgery as an option to me or offered to refer me to an orthopedist. So don’t assume a discussion of surgery will necessarily be a part of usual rheumatology care.
You might also like to read:
Hard truths on RA surgery
8. What’s the grimmest truth about RA surgery?
Over the past few years, as I talked with my orthopedists about which surgeries might help various joints, I was surprised most by this one thing. One of them told me that he hasn’t seen any new surgical options in his specialty for people with RD in decades. Often, surgeries in RD do not actually repair structures as they do for the same “injuries” in other patients.
9. Why do fewer people get RA surgery now?
There is a theory that fewer people with RD are having surgery because the newer medications have worked miraculously so that surgeries are not needed. The answer is actually more complex. Surgeries are delayed because there is a longer list of medication options to try, as well as physical therapies or assistive devices, especially with milder RD. But my doctor has also learned by experience that surgery is not necessarily the best option with unrelenting RD. For that reason, he’s reluctant to operate too quickly in my case.
10. What’s the hardest part about RA surgery?
The hardest part for me of living with a cast on one arm is that the rest of my joints are still very limited, so it’s hard to manage. It’s also frustrating trying to explain why I had surgery to repair two of 200 damaged joints.
WHAT ARE YOUR QUESTIONS ABOUT RA SURGERY? DO YOU HAVE ANY ADVICE TO SHARE?




Thank you for sharing your story about RD surgery. I have had RD for 12 years. I am trying to decide if surgery would be an option for my knee. I appreciate your thoughts and experience.
I have had RA for 54 years since childhood, and under the same group of Rheumatologist group.
Many knee surgeries. A reconstruct when I was 16. My left knee had nothing in it but I held out on knee replacement until 2010. Best thing I ever did. The key is that you do your homework on getting the best orthopedic surgeon. It is a big surgery so make sure you prepare yourself mentally for the process of healing.
Thea:)
KELLY, IT IS SO GOOD TO SEE YOU ON THE RELATIVELY “ACTIVE” LIST AGAIN…SO SORRY YOU HAVE HAD SUCH A ROUGH TIME! HOPE RECOVERY WILL GO QUICKLY, AND THE MENDING WILL BE SUCCESSFUL!
I SLIPPED AND FELL IN THE HOUSE AND BROKE MY RIGHT SHOULDER 3 WEEKS AGO, AND I SO SYMPATHIZE WITH YOU—THE DISCOMFORT, AND INABILITY TO DO MUCH THAT I USED TO DO DAILY,
IS NOT FUN–TO SAY THE LEAST! BUT, AS THE CLICHE GOES, ONE DAY AT A TIME! TAKE CARE, AND WE WILL ALL HOPE FOR BETTER DAYS AHEAD! GENTLE HUGS…..VI
In all four of my joint Replacements, five if you count my right shoulder twice, I have found that a total replacement is much less painful than just getting a repair. When I had my first need done I knew coming out of the or that the pain was gone. The post-surgical pain was almost nothing compared to the pain I had had before surgery. The two shoulder surgeries on my right shoulder both were painless after surgery due to a good combination of pain and nerve meds. The only reason I had to redo it is because my rotator cuff tour and I could no longer lift my arm. The shoulder worked great I just couldn’t use it! Whenever you are thinking about having surgery, just make sure you ask lots of questions. When preparing for my second replacement in the shoulder I asked him if he was going to go in and repair my cough but got in there and it was not repairable would he just do a replacement. He then did some research and we scrapped the hole repair idea and just went for the replacement.
Here’s to a speedy recovery Kelly. Hope it brings you some relief. I am almost two months post double fusion on my neck and while RD wasn’t exactly the cause it did complicate it some. I have been off my RD meds for almost three months but hoping to restart next week. Here’s to easier days ahead for all those who suffer with this disease. Warrior Strong.
As I sit here with my right foot propped up one week post surgery and nine weeks to go, I am happy you published the list. I do believe I am the captain of my own ship when it comes to surgery. However, I believe Sheryl is admiral, she drives me around after all.
Sheryl sounds awesome, Rick.
Heal quickly!
Hi Rick – I am having surgery on my right foot ( fusion of big toe / clean out) on March 4. I am very apprehensive. I have RA ( diagnosed in 1978 at age 26) . Both feet are affected, but am going with the most painful first. Hope your recovery goes smoothly. Also, thank you for the info, Kelly!
Haven’t had to consider surgery just yet. Does not sound like fun. Hope you heal up from it fast. Be well, Kelly…
Thanks, José. I was sure the day would never come.
Absolutely fantastic post, Kelly — it’s so nice to see you writing again! Thank you for the very comprehensive answers about RA surgery, definitely very useful. I can add one thing about joint replacement surgery. I had both hips replaced when I was 16 and I still remember the absence of pain. Which is not to say that it didn’t hurt — of course it hurt. Any time you get cut open, it will hurt. But it was just surgery pain and one of the great things about surgery pain is that it gets a little better every day. There was no more pain in my hips, though, and the recovery was actually pretty quick. I can imagine that that’s only improved in the past 40 years. (OMG, it’s been 40 years…).
I have had both knees replaced and did well. I did have to go off my Rituxin infusions and Leflunomide and my RA really flared. I have degenerative spine disease and neurosurgeon won’t touch me because I have RA. He said it would do more harm than good. I need surgery on both feet and saw an orthopedic surgeon. He was going to fuse bones in my feet which had dislocated and were causing calluses on the soles of my feet. One came open and got infected which put me in the hospital for IV antibiotics. While waiting for that to heal so I could have the surgery, I was diagnosed with PMR (poly myalgia rheumatica) and went through 6 months of high doses of Prednisone. So my RA continued to destroy. I also need surgery to fuse joints in my hands. My right thumb is totally disjointed and facing my left. Now I am back on Rituxin and Leflunomide and my rheumatologist does not want me to have surgery.
I wish you the best on recovery from your hand surgery. Thank you for all you do. It is nice to share with others who understand what we go through.
Among the thousands of things I could say about the usefulness and awesomeness of this post, one thought makes me ROFL. (For those who don’t know me, and/or Kelly, this is a JOKE, an ironic parroting of something ignorant people say to RD patients):
Looking at that photo, all I can say is “Gee, you don’t LOOK sick!”
You continue to amaze …
Thanks for sharing Kelly. I wish you a speedy recovery and sending you a much deserved gentle hug.
I too am soon to be undergoing a fusion on my left hand after a failed ulnar head resection. All I wish for is the pain to stop, of course like you it is my left hand and I am left handed. Once that heals I have to have surgery on the right hand all due to RD. It is so comforting to know with this great site you created that we aren’t facing the challenges alone.
Thank you!
I’m so sorry you have to go through this. Wishing you a successful and speedy recovery. As difficult as it is, if it helps with pain, it’s worth it. Thanks for sharing and all you do for the ra community. You truly are a blessing.
My ra surgery experience was due to a ruptured posterior tibial tendon. It was diseased and I’m guessing steroids played a big role. The ortho couldn’t find the end. Thank God I got a second opinion. The podiatrist wanted to do a cadaver graft in her facility. There wouldn’t have been anything there!
The ortho made me do a slow wean off the prednisone before he would operate. I had 3 different incisions, a plug in the navicular bone, 2 screws and the heel bone cut. He didn’t want an infection and needed the bones to heal. I had to stop injections for a few weeks. I wound up flaring from head to toe. It’s very difficult when you can’t bear weight and the ra is impacting hands, shoulders…
Partial recovery took well over a year and lots of pt. I’m not sure I every really came out of the flare. Although I’m limping, I’m grateful for the days I’m able to walk.
Wishing you all the best out come with your decisions and as pain free a day as possible.
Thanks again, Kelly! Your insight is priceless.
I had to have surgery on my right Achilles tendon due to it shortening from RA. As you know Kelly I have used a power chair full time for years. Due to not being able to walk any distance the tendons in my feet and ankles love to play games. Surgery recovery went well and I can once again pull my toes fairly well. Good to see you back on your blog!